Predetermination Vs Prior Authorization- The Difference
- Prior Authorization
- OneMed Billing


Certified Coders
Specialty Expertise
Clean, Compliant Claims
30+ Specialties Served

30+ Specialties Served
30+ Specialties Served
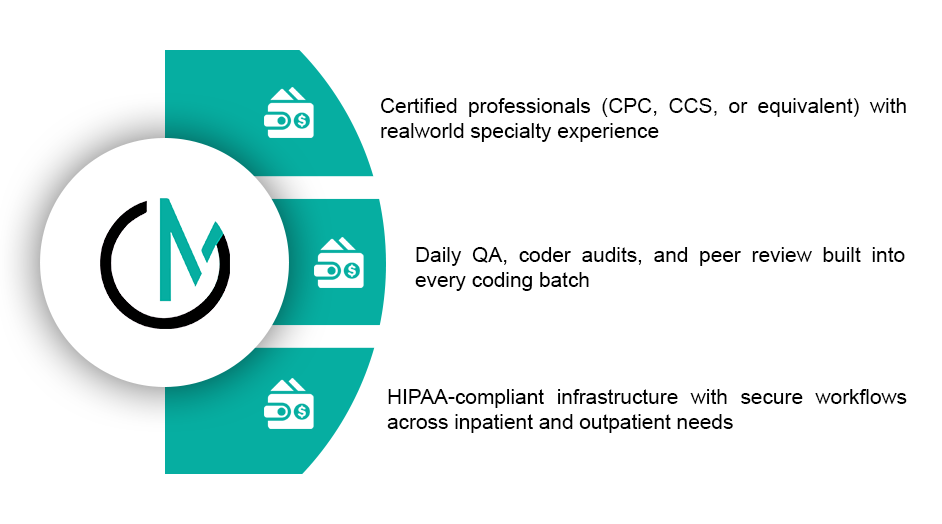
Incorrect or incomplete coding leads to delayed payments, rejected claims, and compliance risks. Many practices struggle to keep up with frequent code updates and payer-specific rules.
Our certified coders handle everything, from diagnosis and procedure coding to modifier assignment and documentation validation, ensuring each claim is accurate, justified, and payer-ready.
We help you code confidently, submit clean claims, and get paid without costly delays.

Whether you need daily coding support or help with backlog cleanup, we deliver reliable coding for all medical specialties.

.
.
.
.
.
We align our coding process with your existing EHR, templates, and documentation style. Whether you prefer coding directly in your billing system or document transfers via SFTP or cloud tools, we adapt to your setup. Our turnaround is fast, most batches are completed within 24–48 hours, and we offer customized workflows for high-volume or same-day coding needs, all backed by ongoing quality audits and coder feedback loops.

Claim denials due to coding
Average coding turnaround
Coding accuracy rate
Compliance audit risk
11%
3+ days
89%
Moderate to high
3%
Under 48 hours
98.7%
Low
“Our claims used to bounce back with coding issues weekly. After switching to OneMed, denials
dropped and reimbursements sped up noticeably.”


You’ll receive detailed coding performance report including completion logs, accuracy scores, and compliance summaries. Our team also provides documentation feedback and recommendations to improve coding efficiency, reduce denials, and stay ahead of audits.
Our process is designed for speed, accuracy, and alignment with your team.
Patient visit documentation received
Assigned coder reviews and codes the visit
Quality check performed by senior coder

Codes delivered back or entered into your system
Feedback loop initiated for documentation gaps, if any
We also support E/M audits, backlog cleanup, and special projects.
Patient visit documentation received
Assigned coder reviews and codes the visit
Quality check performed by senior coder

Codes delivered back or entered into your system
Feedback loop initiated for documentation gaps, if any
We also support E/M audits, backlog cleanup, and special projects.
With OneMed, you don’t just outsource coding, you gain a partner who protects your revenue and compliance.
Every batch goes through a second-level review before delivery. We also provide regular QA and reporting.
Yes. All coders are certified through AAPC, AHIMA, or equivalent organizations and have experience in real practice settings.
Our typical turnaround is 24 to 48 hours, depending on volume and specialty.
Yes. We support internal audits, OIG reviews, and help you stay compliant with all major guidelines.
We work with most major systems, including Epic, Athena, eClinicalWorks, and several custom platforms.