Predetermination Vs Prior Authorization- The Difference
- Prior Authorization
- OneMed Billing


Clean Claims on First Submission
Payer-Specific Checks
Lower Rejection Rates
30+ Specialties Served

30+ Specialties Served
30+ Specialties Served
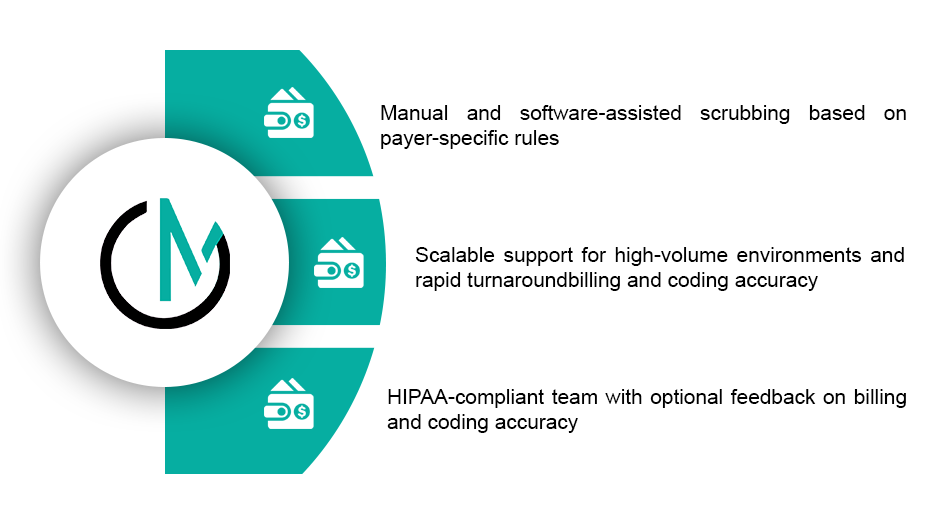
Claim rejections waste valuable time and delay your payments. Most of the time, these issues could have been caught before submission, if someone had reviewed the claim closely.
That’s where we come in. Our team reviews each claim for errors, missing data, and payer-specific rules before it’s ever sent. We catch what automation tools miss and help your practice reduce back-and forth with payers.

Our claim scrubbing process checks every detail of the claim to ensure it meets coding and payer requirements before it reaches the clearinghouse.



We plug into your pre-submission workflow directly, whether claims are sent through your EHR or a clearinghouse. Our team scrubs claims inside Athena, AdvancedMD, DrChrono, Kareo, and others. We offer same day turnaround, real-time alerts on flagged issues, and reports that highlight recurring rejection causes.

Claims rejected at clearinghouse
Time from claim creation to submission
Re-submissions per week
Common rejections missed by software
8%
2 to 3 days
High
Frequent
Less than 1.5%
Same day
Low
High
OneMed catches the issues we didn’t even realize were causing rejections. Our clean claim rate
jumped within the first month.”

We work quickly and thoroughly, reviewing every claim line for possible denials or technical rejections before submission. It’s more than just automation, it’s real people reviewing real claims.

You’ll receive daily claim scrub reports, weekly rejection trend summaries, and real-time alerts when information is missing. We also provide recommendations to reduce repeated errors and optional claim accuracy scorecards to help your team improve over time.
You’ll receive daily claim scrub reports, weekly rejection trend summaries, and real-time alerts when information is missing. We also provide recommendations to reduce repeated errors and optional claim accuracy scorecards to help your team improve over time.
Step
Claim is created in your billing syste
Step
Our team reviews coding, modifiers, and billing data
Step
Payer-specific edits and format rules are applied
Step
Errors flagged, corrected, or returned with comments
Step
Scrubbed claim cleared for submission
Step
Final status documented for reporting
Yes. We offer full rejection handling and can coordinate with your denial team if needed.
Yes. We scrub professional and institutional claims (CMS-1500 and UB-04) across all specialties.
We work with most major platforms, including AdvancedMD, Kareo, Athena, eClinicalWorks, and more.
Claims are typically reviewed and returned within 24 hours — same-day turnaround is available for most practices.
Absolutely. We log every issue and provide trend reports to help your team avoid repeat problems.