What Is An Itemized Bill In Medical Billing?
- Updated Date January 17th, 2026
- Medical Billing
- Follow
Most patients feel confused when they receive a medical bill that doesn’t clearly explain what each charge is for. As healthcare costs continue to rise, more people want to know exactly where their money is going. Billing transparency has become a key part of trust between patients and providers. When a bill is clear and easy to understand, it helps patients feel more confident in their care and allows providers to show honesty in how they handle charges.
Having a detailed, easy-to-understand breakdown of charges can make a big difference. It helps patients feel confident about what they’re being billed for and gives providers a chance to show that their billing process is clear and accurate.
In this blog, you will discover:
- What is an Itemized Bill in Medical Billing?
- Why an Itemized Bill Matters in Medical Billing?
- What Makes an Itemized Bill Different from Others?
- What Information Appears on an Itemized Bill?
- When to Use an Itemized Bill?
- How to Request an Itemized Bill?
- Conclusion
What is an Itemized Bill in Medical Billing?
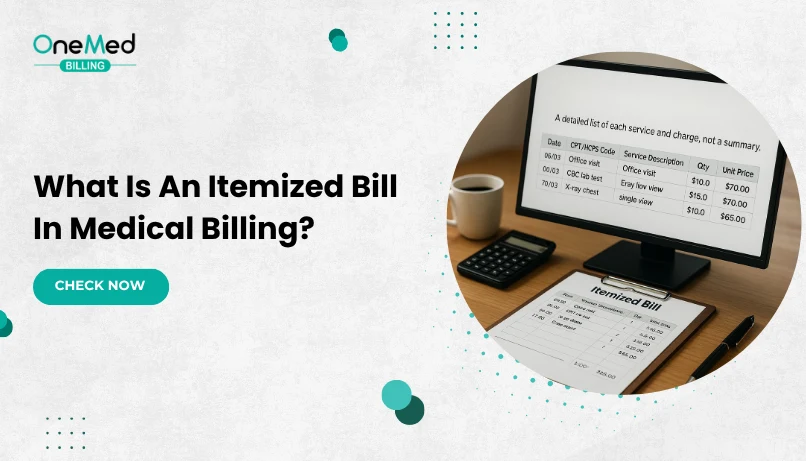
An itemized bill in medical billing is a detailed statement that breaks down every service, test, medication, and supply used during a patient’s visit. Instead of showing just one total amount, it lists each charge line by line, along with important details such as the date of service, department, and the codes used to identify each procedure or diagnosis.
This level of detail allows patients to see exactly what they are paying for and helps providers maintain accuracy when submitting claims to insurance companies. Each line typically includes a CPT or HCPCS code for the service provided and an ICD-10 code that explains the reason for that service.
Why an Itemized Bill Matters in Medical Billing?
An itemized bill is a detailed record that helps patients understand what they are being charged for and why. It keeps the billing process clear, fair, and easy to trust for everyone involved.
When patients receive a detailed breakdown of every charge, they can understand where their money is going. This helps them feel more informed and less frustrated when it’s time to pay.
Here are a few important reasons why itemized bills matter:
1. They Help Catch Billing Errors
Sometimes charges are added by mistake. An itemized bill lets patients check each line and speak up if something doesn’t look right.
2. They Improve Patient Trust
Clear billing shows that your office is open and honest. It helps patients feel respected and more likely to return for care.
3. They Make Insurance Processing Easier
Insurance companies often ask for detailed billing information. An itemized bill gives them what they need to review claims and process payments faster.
4. They Reduce Disputes and Confusion
When patients can see the cost of each service or supply, they are less likely to question the total amount or feel surprised by the bill.
By giving patients an itemized bill, your office shows that it values accuracy, fairness, and clear communication.
What Makes an Itemized Bill Different from Others?
Medical billing comes with a lot of paperwork, and it’s easy for patients to get confused. That’s why it’s helpful to explain how an itemized bill is different from other common billing documents. Each one serves a unique purpose, and knowing the difference helps patients understand their medical charges more clearly.
Itemized Bill vs Summary Bill
A summary bill gives a quick overview of what the patient owes. It usually includes the total cost of care, any insurance payments, and the final balance due. What it doesn’t show are the details behind each charge.
An itemized bill, on the other hand, lists every service, procedure, supply, and medication with a description and cost. While the summary bill tells the patient how much they owe, the itemized bill tells them why they owe it.
Itemized Bill vs Explanation of Benefits
An Explanation of Benefits (EOB) is not a bill. It’s a document sent by the patient’s insurance company that explains how a claim was processed. It shows what the provider charged, what the insurance paid, and what the patient may still owe.
The itemized bill comes from the provider, not the insurer. It’s a request for payment and includes detailed pricing. The EOB is for reference only and may not match the provider’s charges exactly, but it helps patients compare and verify the costs.
Itemized Bill vs UB-04 and Superbill
The UB-04 is a billing form used mainly by hospitals and other large facilities to bill insurance companies. It includes codes and other technical details that aren’t always useful for patients.
A superbill is a detailed invoice used in outpatient care or private practices. It includes services provided and codes used for insurance billing, but it’s mostly designed for providers and insurance, not for patient review.
What Information Appears on an Itemized Bill?
An itemized bill is a detailed list of charges. It’s a complete record of the medical services a patient received, supported by the billing and coding details that explain each charge. Every line on the bill represents a specific service, procedure, supply, or medication used during treatment. Understanding what appears on it helps both patients and providers verify accuracy, confirm insurance coverage, and prevent costly errors.
Core Details
The first section of an itemized bill contains key information that identifies the patient, provider, and visit details. These basics set the foundation for the billing record and ensure that every charge is tied to the right encounter.
Here’s what you’ll usually find under the core details section:
- Patient Information: Name, address, account number, date of birth, and insurance ID.
- Provider Information: Name of the physician, clinic, or hospital that delivered the care.
- Dates of Service: The specific dates when tests, procedures, or consultations took place.
- Department or Location: The area where the service was provided, such as emergency, radiology, or lab.
- Billing Reference Number: A unique internal ID used by the billing team to track the account.
These basic identifiers help ensure that billing data lines up with the patient’s medical record, claim forms, and insurance policy. If any of this information is incorrect such as a missing service date or wrong provider, it can cause claim denials or payment delays.
When to Use an Itemized Bill?
An itemized bill is most helpful when a charge seems high or unfamiliar, or when the total does not match your Explanation of Benefits (EOB). It lists each service, quantity, and price so you can confirm what was done and catch mistakes before paying. It is also useful after a denial or partial payment, for out-of-network visits or facility fees, and when arranging a payment plan or applying for financial assistance. Many patients request one to use HSA or FSA funds and to keep clear records for taxes.
How to Request an Itemized Bill?
Every patient has the right to an itemized bill. To request one, contact the billing office by phone, email, or through your patient portal. Share your name, date of birth, account or claim number, and the dates of service. Ask for a line-by-line bill with plain-English descriptions and the related codes. You can choose how to receive it (email, mail, or portal upload). If you’re reviewing charges, ask the office to place the account on hold so no late fees or collections start during the review.
Conclusion
An itemized bill is a detailed billing document. It’s a vital part of clear, accurate, and honest healthcare communication. When patients can see exactly what they’re being charged for, they feel more informed, more in control, and more confident in the care they receive.
For clinics and healthcare providers, offering itemized bills is a step toward building stronger relationships with patients. It reduces billing confusion, helps resolve disputes faster, and shows that your office values fairness and transparency.
Encourage patients to ask questions, request itemized bills when needed, and take an active role in reviewing their medical costs. It’s a small change that leads to better experiences for patients.
Frequently Asked Questions
Find quick answers to common questions about this topic, explained simply and clearly.
Why should you ask for an itemized bill?
To see each service, quantity, and price. It helps you spot mistakes, compare with your EOB, and ask clear questions before paying.
Who typically provides itemized bills?
Your provider’s billing department or hospital billing office. You can request it by phone, email, or through the patient portal.
Can I dispute charges on an itemized bill?
Yes. Contact the billing office with the account number and the exact line in question. Ask for a review and a corrected bill or a written explanation.
What is an itemized bill example?
A line-by-line list, such as: Office Visit, CPT 99213, Qty 1, Unit $120, Total $120 CBC Lab Test, CPT 85025, Qty 1, Unit $35, Total $35 Injection, CPT 96372, Qty 1, Unit $25, Total $25 Subtotal