Predetermination Vs Prior Authorization- The Difference
- Prior Authorization
- OneMed Billing


Accurate Payment Matching
Real-Time Posting
Clear Financial Reporting
30+ Specialties Served

30+ Specialties Served
30+ Specialties Served
When payments are posted late or incorrectly, it slows down follow-up,
skews reports, and hides revenue problems until it’s too late.
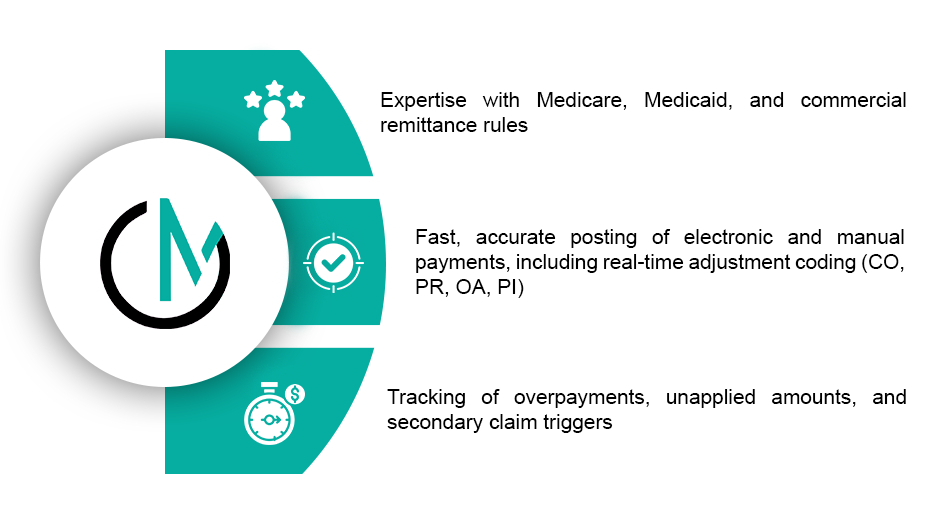
Our team handles both manual and electronic remits with precision
matching payments, entering adjustments, and flagging variances. We
help you stay on top of your collections, reduce unposted revenue, and
spot issues faster.
You get complete visibility and cleaner financials without the backlog.

From ERA to EOB, we handle every detail so your billing team can stay focused on recovery and reporting.






We work directly within your billing platform, whether it’s Athena, eClinicalWorks, Kareo, or a custom EHR, and post payments just as your in-house team would. ERA files are imported from clearinghouses, manual EOBs are processed with payer-specific coding, and scanned documents from lockbox or paper sources are handled securely. Every posting batch is logged, and custom remittance reports can be delivered in your preferred format.

Appeal win rate
Time to file appeal
Monthly recovered revenue
Denials written of
39%
5 to 7 days
Low
Frequent
76%
1 to 2 days
Consistent growth
Reduced significantly
OneMed brought structure and accuracy to our posting. Now we know what’s paid, what’s
pending, and what needs action, without chasing down old batches.”

Whether you post hundreds of claims a day or manage multiple payment sources, we scale with your needs. Our team is trained in payer-specific codes, contractual rules, and how to handle discrepancies professionally.

We give you clear, accurate numbers to base your decisions on, not estimates or assumptions. You’ll receive daily payment logs, denial and adjustment breakdowns, reconciliation summaries by batch, and custom reports built around your billing structure. Refunds, reworks, and write-offs are all flagged so you can take action fast.
We post payments with discipline, each step focused on clean data and fast turnaround.
Step
ERA or EOB received
Step
Payment matched to patient and DOS
Step
Adjustments and denials posted by line item
Step
Balance routed to secondary or patient, if needed
Step
Batches reconciled and reports sent
Step
Any issues flagged for billing team review
With OneMed, posting is not just data entry, it's the financial clarity your team needs to keep collections strong and follow-up focused.
We balance each batch against deposit totals and provide detailed reports with any discrepancies flagged.
Yes. We post all types of payments and clearly separate patient responsibility.
We typically post ERAs within 24 to 48 hours of receipt.
Absolutely. We support manual posting from physical documents or scanned PDFs.
It is the process of recording insurance and patient payments in the billing system to keep accounts accurate and up to date.