Predetermination Vs Prior Authorization- The Difference
- Prior Authorization
- OneMed Billing


Accurate Data Capture
Clean Claim Submissions
Faster Revenue Flow
30+ Specialties Served

30+ Specialties Served
30+ Specialties Served
Small mistakes in charge entry lead to big problems, denied claims,
underpayments, and rework for your billing staff. When you’re
managing hundreds of encounters each week, it only takes one missing
field to slow everything down.
We step in to make sure your charges are entered accurately, coded
correctly, and double-checked before submission. You get clean claims
and a faster revenue cycle without the manual hassle.

Our charge entry specialists review every detail to make sure your claims go out right the first time.

Patient demographics, insurance info, and eligibility validation
CPT, ICD-10, HCPCS, POS, and modifier entry
Units, provider, rendering, and facility info
Detection of bundled/unbundled charges and reconciliation with appointments
Submission readiness checks and final QA
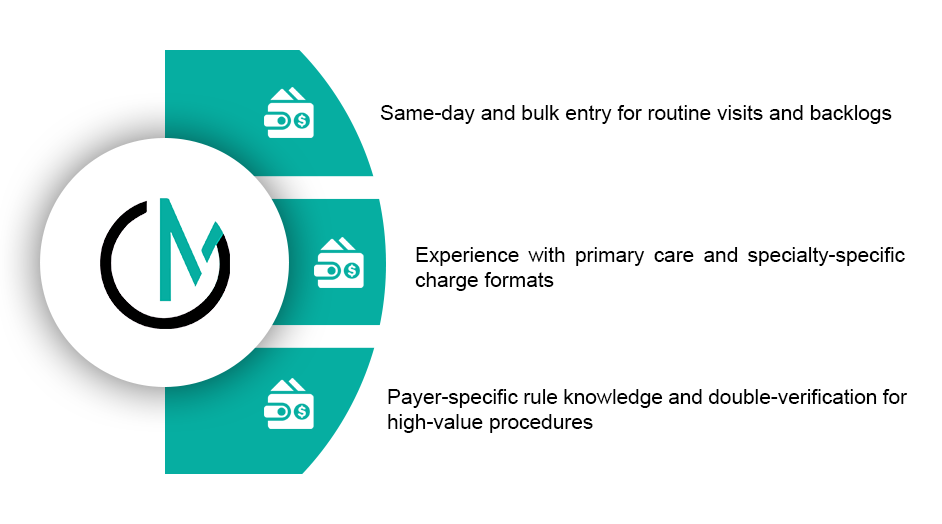
We match our process to your system, whether you use Athena, eClinicalWorks, AdvancedMD, or another platform. Our team can post charges directly into your system or process batches via HL7 or secure file transfers. We validate data in real time, provide same-day entry for routine encounters, and collaborate with your team on any missing or conflicting information to avoid delays

Claims held for missing data
Data entry errors per 100 claims
Time from visit to claim submission
Denials due to charge entry issues
9%
7
3 to 5 days
Frequent
1.5%
Under 1
Same day or next day
Rare
“With OneMed’s charge entry support, our team no longer has to double-check every claim. Their
accuracy saves us time and reduces denials.”

Whether you're processing a few dozen encounters a day or managing multiple providers across locations, we scale with your needs. Our team works quickly and carefully to keep your claims moving without delays.

You’ll receive complete visibility into charge entry performance through daily logs, reconciliation reports, and error summaries. We flag conflicts, recommend fixes, and optionally provide feedback on missing documentation or coding gaps to help you maintain a clean and timely submission process.
Every charge goes through a consistent and reliable process to ensure submission-ready results.
Chart or charge sheet received
Patient and payer data validated
CPT, ICD, and modifiers entered

Claim reviewed for completeness
Entry saved and logged for QA
Report sent to your team
Chart or charge sheet received
Patient and payer data validated
CPT, ICD, and modifiers entered

Claim reviewed for completeness
Entry saved and logged for QA
Report sent to your team
With OneMed, charge entry is not just data input, it’s the foundation of a healthy revenue cycle.
Absolutely. We scale our team based on your encounter volume and provider count.
We work with most major EHRs and billing platforms, including AdvancedMD, Kareo, Athena, DrChrono, and others.
Yes. For scheduled visits, we complete charge entry within 24 hours — often the same day.
We use a two-step review process that includes code validation and demographic checks before saving.
Yes. We offer integrated coding services or can coordinate with your in-house coder if needed.