Predetermination Vs Prior Authorization- The Difference
- Prior Authorization
- OneMed Billing

Strong Appeal Letters
Faster Reversals
Lower Write-Off Rates
30+ Specialties Served

30+ Specialties Served

30+ Specialties Served
When denials go unchallenged, you're not just losing revenue, you're
missing out on money your practice has already earned. Most denied
claims are preventable or appealable, but many teams don’t have the
time to handle them properly.
Our team takes over your appeals queue. We review each denial,
gather documentation, write payer-specific appeal letters, and follow
through until the claim is resolved.
We turn denied claims into recovered income.
From initial denial analysis to final resolution, we cover everything needed to give each claim the best chance of approval.

Review of denial codes and claim data

Categorization of appealable vs. non-appealable denials
Creation of detailed appeal letters with supporting evidence.
Submission via portal, fax, or mail with tracking and resolution follow-up.

Peer-to-peer support, provider coordination, and audit logs
We support most major billing platforms and clearinghouses. Denials are handed off via batch files, email, or portal. We coordinate with your internal coders or billers as needed, and we share real-time appeal status updates while tracking all documents securely.
Appeal win rate
Time to file appeal
Monthly recovered revenue
Denials written of
39%
5 to 7 days
Low
Frequent
76%
1 to 2 days
Consistent growth
Reduced significantly
Our appeals were inconsistent, and many denials just sat in the system. Since partnering with
OneMed, we’ve recovered thousands in claims we thought were lost.”

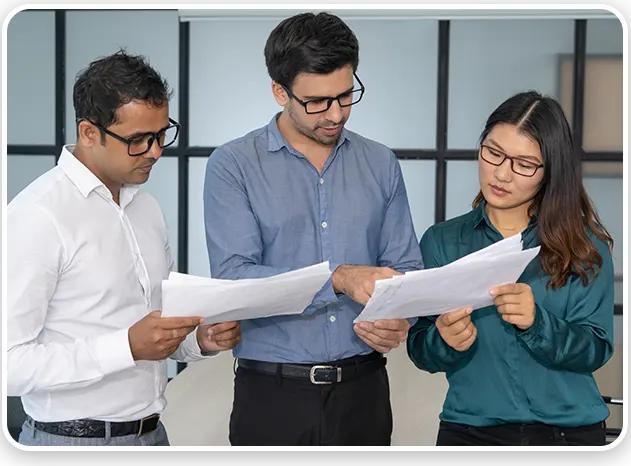
We handle complex appeals that require more than a templated letter. Our team supports cases involving prior authorization, medical necessity, and coding-related denials. We coordinate with providers for peer-to-peer reviews or clinical documentation when needed, and we customize every appeal based on the specific language and expectations of the payer. Whether you're dealing with Medicare, Medicaid, or commercial plans, we have experience across all major specialties, including behavioral health, infusion, DME, and surgical services.
We provide full visibility into every appeal submitted, including details, follow-ups, and outcomes, so you never have to guess


We move each denied claim through a clear path from problem to payment.
Step
Denial is received and reviewed
Step
Root cause and appeal eligibility determined
Step
Appeal letter created and documentation gathered
Step
Submission completed with tracking
Step
Follow-up with payer begins
Step
Final status updated in logs and reported to your team
We don’t just log referrals, we manage them from start to finish.
Yes. Every appeal is tracked through to resolution, and results are logged and reported.
Yes. We create custom letters and submit them based on the payer’s preferred method (portal, fax, or mail).
Absolutely. We coordinate with providers for documentation and can support peer-to-peer processes.
We manage appeals for Medicare, Medicaid, and commercial payers across all 50 states.
Most appeals are submitted within 24 to 48 hours after denial review.