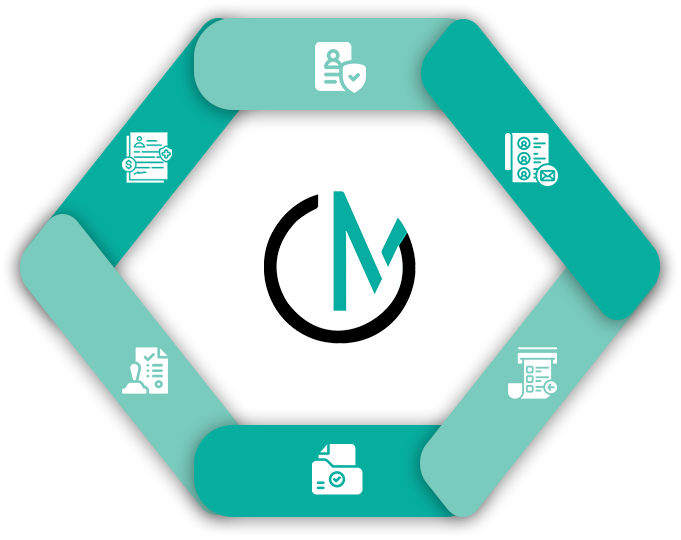
Predetermination Vs Prior Authorization- The Difference
- Prior Authorization
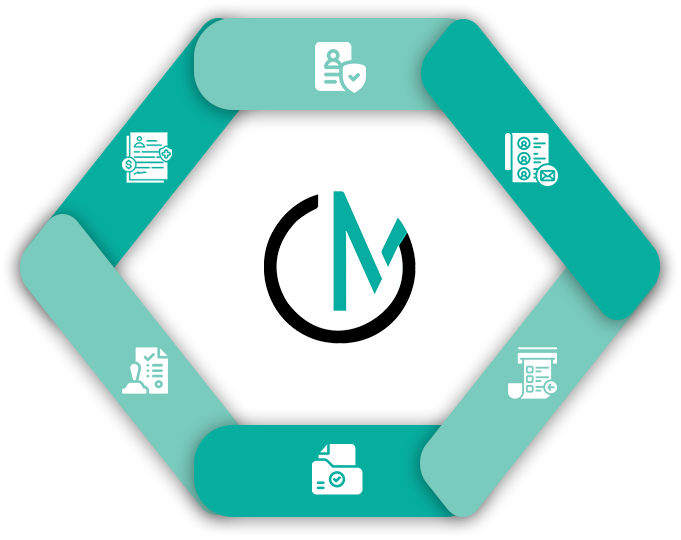
- OneMed Billing


Shorter Wait Time
Accurate Data Entry
Fewer Claim Errors
30+ Specialties Served

30+ Specialties Served
30+ Specialties Served
Patient registration is one of the most important steps in the revenue
cycle. When it’s rushed or incomplete, it leads to claim errors, delayed
payments, and frustrated patients.
We step in to support or fully manage your registration process, collecting accurate demographics, insurance details, and referral
information before the visit. Your team gets more time to focus on care,
not data entry.

Whether you need help with new patients, pre-registration, or same-day walk-ins, we’ve got you covered.
We collect and enter accurate patient information, including insurance plan details.

Our team verifies coverage, plan benefits, and confirms active status before the visit.

We intake and review referrals or pre-authorizations required by payers.
We manage primary and secondary insurance coordination, and check co-pays, deductibles, and patient responsibility.
Final verified information is securely handed off in real time to your billing or scheduling team.

You don’t need to overhaul your system or retrain your staff. We integrate directly into your EHR or practice management software using your current process. Registration can be handled remotely through calls, emails, or your patient portal. We start pre registration 24 to 72 hours before the appointment and handle same-day entries as needed. Our team can work live in your system or securely hand off completed data based on your preference. Everything is tailored to your schedule, protocols, and specialty
Claims denied due to registration errors
Average patient check-in time
Patient data entry accuracy
Claim holds due to missing info
14%
12 minutes
86%
Frequent
Under 3%
5 minutes
98.5%
Rare
“Our front desk used to scramble during peak hours. With OneMed managing pre-registration, we have fewer delays and our claims are going through cleaner than ever.” 
We support practices of all sizes, from solo providers to large, multi-site networks. Our team has experience handling front end registration for family medicine, specialty care, behavioral health, and diagnostic clinics. We understand the nuances of Medicare, Medicaid, and commercial payer rules and apply verification workflows based on the insurance type and location. Our infrastructure is fully HIPAA-compliant, and we assign dedicated agents who work exclusively with your practice for consistency and accountability

We move every patient through a consistent intake flow that sets your billing team up for success.
Patient information received (via form, call, or referral)
Demographics and insurance details collected
Eligibility and benefit checks completed
Authorization or referral requirements noted
Confirmation sent to front desk or billing
Final records saved or submitted based on your system
Patient information received (via form, call, or referral)
Demographics and insurance details collected
Eligibility and benefit checks completed
Authorization or referral requirements noted
Confirmation sent to front desk or billing
Final records saved or submitted based on your system

We keep your front office and billing teams updated with detailed registration logs and real-time alerts. If any information is missing or mismatched, you’re notified right away. We also provide verification results with payer-level detail and track the status of referrals and authorizations. Weekly summaries highlight overall performance and suggest improvements to optimize your intake process further
We help you avoid rework, reduce denials, and improve patient satisfaction from the very first step.
Yes. We begin the registration process 24 to 72 hours before the visit, depending on your schedule and volume.
We work with most major systems including Athena, Kareo, eClinicalWorks, and more.
Yes. Our process includes complete eligibility and benefits checks for every scheduled patient.
Absolutely. All staff are trained in HIPAA and work on secure systems with full access controls.
Yes. We handle same-day registrations and flag incomplete data before claims are submitted.