What Is Denial Management In Medical Billing?
- Updated Date Jan 22, 2026
- Denial Management
- Follow
Claim denials are one of the biggest hidden reasons providers lose revenue, not because the services were wrong, but because the process breaks somewhere between registration and payer rules. Every denied claim is money you already earned but haven’t collected yet, and most denials are preventable when you know exactly where they come from and how to fix them fast.
What is denial management in medical billing?
Denial management in medical billing is a structured, provider-side process used to identify, analyze, resolve, and prevent insurance claim denials in order to protect revenue and maintain a healthy revenue cycle.
From a practical RCM perspective, denial management is not just about appealing denied claims. It covers the entire lifecycle of a denial, including:
- Detecting denials from ERA/EOBs
- Understanding why the payer denied the claim
- Taking the correct action (correct & resubmit, appeal, or write-off)
- Fixing the root cause so the same denial does not happen again
For providers, effective denial management directly impacts cash flow, accounts receivable (A/R), net collections, and operational costs.
How does denial management work in actual live workflows?
In real provider environments, denial management is not a one-time task, it is a continuous, system-driven workflow that runs alongside daily billing and A/R operations. The goal is to resolve denials quickly without disrupting claim throughput and to prevent the same issues from recurring.
Below is how denial management typically works in live medical billing workflows.
1. Denials are identified through ERA/EOB posting
The workflow starts when payers adjudicate claims and send ERA (Electronic Remittance Advice) or paper EOBs. During payment posting:
- Claims with zero or partial payment are flagged
- CARC and RARC codes indicate the denial reason
- Denied claims are automatically or manually routed to a denial workqueue
At this stage, speed matters, early identification protects appeal timelines and timely filing limits.
2. Denials are categorized and normalized
Once captured, denials are classified in a standardized way, usually by:
- Payer
- Denial category (eligibility, authorization, coding, medical necessity, timely filing, etc.)
- Root cause (front-end error, coding issue, documentation gap, payer policy)
This step is critical because raw payer denial codes vary widely. Most mature billing teams map payer-specific codes into internal denial categories so trends can be tracked accurately.
3. Denials are prioritized based on recovery value
Not all denials receive equal attention. In live workflows, teams prioritize based on:
- Dollar value of the claim
- Proximity to appeal or filing deadlines
- Payer-specific overturn likelihood
- Contractual or compliance risk
High-dollar and time-sensitive denials move first, while low-value or non-recoverable denials may be deprioritized or written off according to policy.
4. Denials are routed to the correct owner
Effective denial management depends on clear ownership. In practice:
- Eligibility or demographic denials go to front-end or eligibility teams
- Coding denials go to certified coders
- Medical necessity denials go to clinical documentation or HIM
- Authorization denials go to prior auth teams
- Appeals go to specialized denial or appeals staff
This prevents billing teams from wasting time on issues they cannot correct.
5. Correct-and-resubmit or appeal actions are executed
After review, the team takes one of three actions:
- Correct and resubmit (for fixable errors like missing modifiers or demographics)
- Appeal the denial (for medical necessity, policy misapplication, or documentation disputes)
- Write off (for non-covered services or contractually denied claims)
For appeals, supporting documentation is gathered, payer-specific appeal formats are followed, and submissions are tracked to completion.
6. Outcomes are tracked and posted
As payers respond:
- Payments or adjustments are posted
- Appeal outcomes are logged
- Remaining balances are reassessed
This ensures A/R remains accurate and prevents denied claims from aging indefinitely.
7. Root-cause insights feed denial prevention
The final and most overlooked step is closing the feedback loop. Denial data is analyzed to:
- Identify top denial reasons by payer, location, and specialty
- Fix front-end intake gaps
- Update coding and documentation guidelines
- Adjust claim edits and scrubber rules
- Train staff using real denial examples
This step turns denial management from a reactive function into a proactive revenue protection strategy.
Difference between a denied claim and a rejected claim
In medical billing, the terms denied claim and rejected claim are often used interchangeably, but they represent two very different outcomes in the claim lifecycle. For providers, understanding this difference is essential because each requires a different resolution approach, affects payment timelines, and has a direct impact on accounts receivable and revenue recovery.
Below is a clear and practical comparison to help billing teams take the right action at the right time.
|
Aspect |
Rejected Claim |
Denied Claim |
|
When it occurs |
Before payer processing |
After payer processing |
|
Where it happens |
Clearinghouse or payer intake |
Insurance payer |
|
Claim status |
Not adjudicated |
Adjudicated |
|
Payment decision |
No payment decision made |
Payment denied or reduced |
|
Main cause |
Missing or invalid data |
Coverage, policy, or medical rules |
|
Common examples |
Invalid insurance ID, missing NPI, formatting errors |
No authorization, medical necessity not met, timely filing |
|
How to fix |
Correct errors and resubmit |
Appeal or correct and resubmit |
|
Appeal required |
No |
Often required |
|
Impact on A/R |
Minimal if corrected quickly |
Higher A/R impact if not managed |
|
Best prevention |
Front-end data validation |
Strong denial management process |
Key takeaway:
- Rejected claims fail basic validation checks and never reach payer adjudication.
- Denied claims are processed by the payer and formally not paid.
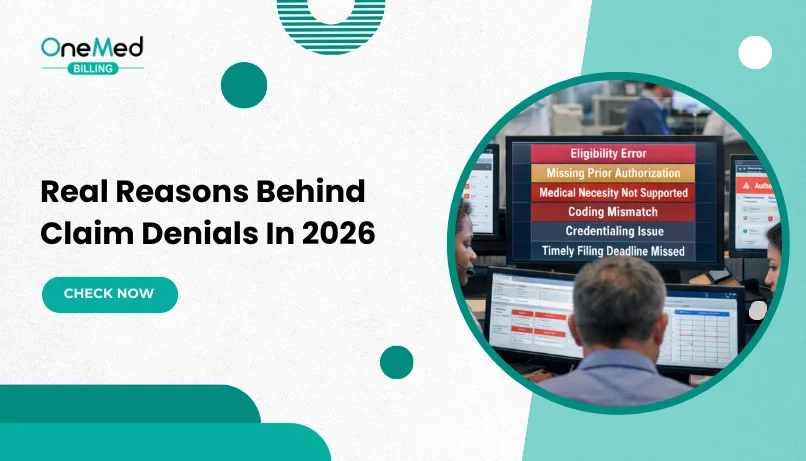
Common claim denial reasons in medical billing
Claim denials are rarely “random.” For most providers, denials come from a small set of recurring issues across the revenue cycle - front-end registration, eligibility checks, authorization workflows, coding, documentation, and payer filing rules. Knowing the most common claim denial reasons helps billing teams spot patterns faster, prioritize fixes that prevent repeat denials, and improve clean claim rates, cash flow, and A/R performance.
Eligibility and coverage denials
These denials occur when the patient’s insurance coverage is inactive, terminated, or does not cover the service on the date of service. They are usually caused by incomplete or outdated eligibility verification and incorrect subscriber information at registration.
Prior authorization and referral denials
Payers deny claims when required prior authorizations or referrals are missing, expired, or do not match the billed services. These denials often have low recovery rates and highlight gaps in authorization tracking and documentation.
Coding and modifier denials
Coding-related denials happen due to incorrect CPT or ICD codes, missing or invalid modifiers, unbundling issues, or NCCI edit violations. They are typically preventable with strong coding reviews and payer-specific coding rules.
Medical necessity denials
These denials occur when the payer determines that the clinical documentation does not support the medical necessity of the services billed. Inadequate provider notes or lack of alignment with payer medical policies are common causes.
Timely filing denials
Timely filing denials result when claims, corrected claims, or appeals are submitted after payer-defined deadlines. These denials are fully preventable with proper claim tracking and deadline management.
While these categories explain where denials originate, the underlying causes often go deeper. Many practices continue to see repeat denials because the same issues show up across different payers and service lines. A closer look at the real reasons behind claim denials helps connect these denial types to broader revenue cycle gaps.
CARC and RARC codes in denial management
CARC and RARC codes play a critical role in denial management by explaining why a claim was denied or underpaid and what action, if any, a provider should take next.
What are CARC codes in medical billing?
CARC (Claim Adjustment Reason Codes) describe the primary reason a payer adjusted or denied a claim. These codes indicate what happened to the claim, such as lack of coverage, missing authorization, or billing errors.
CARC codes help billing teams quickly identify the type of denial and determine whether the claim should be corrected, appealed, or written off.
What are RARC codes in medical billing?
RARC (Remittance Advice Remark Codes) provide additional details or instructions related to a CARC. While CARC codes explain the reason for the denial, RARC codes explain what the provider must do next, such as submitting additional documentation or correcting specific information.
RARC codes often clarify payer expectations and are especially useful during appeals.
In denial management, CARC and RARC codes are used to:
- Route denials to the correct team (billing, coding, authorization, or clinical)
- Decide between correction, resubmission, or appeal
- Track denial trends by payer and denial type
- Identify preventable denials and process gaps
Most providers map payer-specific CARC/RARC combinations into internal denial categories to standardize reporting and workflow automation.
What steps should you take if a claim is denied?
When a claim is denied, providers need a clear, time-sensitive workflow to recover revenue and avoid repeat denials. The right approach starts with understanding the payer’s reason, then taking the correct action - resubmit, appeal, or write off, while tracking everything to closure and capturing the root cause for prevention.
Review the denial reason on the ERA/EOB
Start by carefully reviewing the ERA or EOB to identify the exact reason the payer denied or underpaid the claim. The denial reason and remark codes explain whether the issue is related to eligibility, authorization, coding, documentation, or payer policy. This step is critical because the next action should always be based on what the payer has specifically cited.
Verify claim and patient information
Before taking any corrective action, confirm that all claim details are accurate. This includes patient demographics, insurance information, dates of service, provider identifiers, place of service, and charge details. Also review CPT, ICD-10, modifiers, and units to ensure they align with payer billing rules. Many repeat denials occur when incorrect information is resubmitted without proper validation.
Determine the correct resolution path
Once the issue is confirmed, decide whether the claim should be corrected and resubmitted, appealed, or written off. Correct-and-resubmit is appropriate for fixable errors such as missing modifiers or demographic issues. Appeals should be pursued when the claim was billed correctly but denied due to policy interpretation or medical necessity. Write-offs should only be used when the denial is truly non-recoverable under payer or contractual rules.
Gather supporting documentation for appeals
If an appeal is required, collect documentation that directly supports the services billed. This may include clinical notes, operative reports, authorization approvals, referrals, and any required payer forms. Focused and relevant documentation increases the likelihood of a successful appeal and reduces back-and-forth with the payer.
Submit and follow up until resolution
Submit the corrected claim or appeal within the payer’s specified timeframe and through the appropriate channel. After submission, actively track the claim status, follow up as needed, and post payments or adjustments promptly once a response is received.
Capture root causes to prevent future denials
After the denial is resolved, document the underlying cause and share insights with the appropriate teams. Use this information to improve front-end verification, authorization processes, coding accuracy, and documentation practices. This final step helps reduce future denials and strengthens overall revenue cycle performance.
How outsourcing medical billing can help with denial management
Outsourcing your billing to a team that offers dedicated denial management services can be the fastest way to stop revenue leakage and stabilize cash flow because denials are handled daily with strict tracking, payer-specific expertise, and clear ownership from start to finish.
Instead of your in-house staff juggling posting, calls, resubmissions, and appeals and missing deadlines in the process, a specialized denial team identifies the true denial reason, fixes and resubmits when appropriate, builds stronger appeal packets when needed, and follows up until the claim is resolved. This helps you recover more revenue, reduce avoidable write-offs, and lower A/R aging. It also reduce future denials by analyzing trends and fixing root causes such as eligibility, authorization, coding, documentation, and payer rule compliance, which means less rework for your staff and more predictable collections.
Conclusion
Denial management is not just about fixing unpaid claims, it is a core revenue protection process for providers. When you understand why denials happen, respond with a clear workflow, and use denial data to prevent repeat issues, you improve clean claim rates, speed up payments, and reduce avoidable write-offs. If your team is stretched or denials are piling up in A/R, partnering with a specialist that provides dedicated denial management services can help you recover more revenue, strengthen appeals, and reduce denial volume over time through consistent follow-up and process improvements.
Frequently Asked Questions
Find quick answers to common questions about this topic, explained simply and clearly.
What is meant by denial management?
Denial management is the process of finding, fixing, and preventing claim denials so providers can recover payments and reduce repeat denials.
What are the steps in claim denial management?
Capture the denial, identify the reason, correct and resubmit or appeal, follow up to resolution, and log the root cause to prevent repeats.
What are the two types of denials?
Soft denials are fixable and recoverable with corrections or documentation. Hard denials are usually non-recoverable, often due to non-coverage or missed deadlines.
What are the most common denial codes?
Common denial codes in medical billing CO-50 - Non-covered services under the patient’s plan CO-97 - Service included in another procedure (bundled) CO-16 - Missing or invalid information on the claim CO-18 - Duplic