12 Most Common Denial Codes and How to Prevent Them
- Updated Date Feb 12, 2026
- Denial Management
- Follow
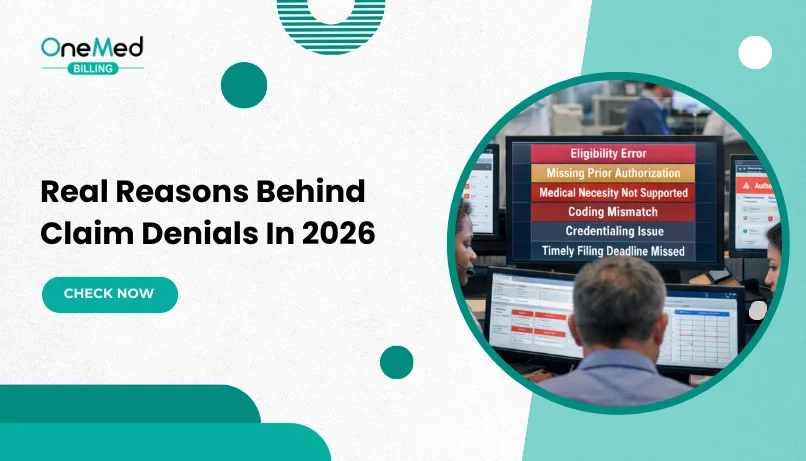
Medical billing denial codes are a major contributor to delayed reimbursements and revenue leakage for healthcare providers. When claims are denied, practices face additional administrative workload, slower cash inflows, and increased pressure on accounts receivable. While denial codes explain how a claim was rejected, they do not always clarify the deeper workflow issues that led to the denial.
Understanding what each code represents, along with the underlying reasons behind claim denials, is essential for identifying recurring process gaps and preventing repeat errors. Effective denial management depends not only on correcting individual claims but also on analyzing patterns, addressing root causes, and strengthening internal controls across the revenue cycle.
Below is a structured, practical list of the most common medical billing denial codes, including their descriptions, root causes, and clear action steps to resolve current denials and reduce future occurrences.
|
Denial Code |
Description |
Primary Cause |
Quick Fix |
|
CO-11 |
Diagnosis inconsistent with procedure |
ICD–CPT mismatch |
Correct diagnosis and procedure coding |
|
CO-16 |
Claim lacks information or has invalid information |
Missing or incorrect claim data |
Review documentation and resubmit |
|
CO-18 |
Duplicate claim or service |
Claim already processed |
Check claim status before resubmission |
|
CO-27 |
Insurance or coverage expired |
Policy inactive on date of service |
Verify eligibility before service |
|
CO-29 |
Timely filing limit expired |
Late claim submission |
Submit within payer filing deadline |
|
CO-50 |
Non-medically necessary service |
Medical necessity not supported |
Submit clinical documentation |
|
CO-96 |
Non-covered charges |
Service not covered by plan |
Verify benefits and authorization |
|
CO-109 |
Claim not covered by this payer/contractor |
Incorrect payer billed |
Confirm primary and secondary insurance |
|
CO-167 |
Diagnosis not covered |
Diagnosis excluded under plan |
Review coverage guidelines |
|
CO-197 |
Precertification/authorization absent |
Missing prior authorization |
Obtain authorization before service |
|
CO-204 |
Service not covered under patient’s benefit plan |
Invalid or missing modifier |
Apply appropriate modifier |
|
CO-B7 |
Provider not credentialed with the payer |
Credentialing not completed |
Complete payer enrollment |
12 Most Common Denial Codes and How to Prevent Them
Below are the 12 most common medical billing denial codes, along with real-world examples and practical steps to prevent them.
1. CO-11: Diagnosis Inconsistent with Procedure
Denial code CO-11 occurs when the diagnosis code submitted on a claim does not support the medical necessity of the billed procedure. The payer determines there is no valid clinical relationship between the diagnosis and the service provided.
Common Reasons for CO-11 Denials
- The ICD-10 diagnosis code does not justify the procedure performed
- Mismatch between provider documentation and coded services
- An incorrect diagnosis selected in the EHR or practice management system
- Insufficient clinical documentation to support medical necessity
- CPT and ICD-10 code combinations not covered under payer policies
- Failure to follow payer-specific Local Coverage Determinations (LCDs)
This denial is frequently seen in specialties such as dermatology, orthopedics, and podiatry, where diagnosis-to-procedure relationships must meet strict payer guidelines.
Example
Submitting a claim for toenail removal (CPT 11730) with a diagnosis of acne (ICD-10 L70.0) will result in a CO-11 denial because the diagnosis does not support the medical necessity of the procedure.
How to Fix a CO-11 Denial
- Review the medical record to confirm the correct diagnosis and procedure
- Update the diagnosis code to accurately reflect the patient’s condition
- Ensure clinical notes clearly support medical necessity
- Correct the claim and resubmit with appropriate documentation
How to Prevent CO-11 Denials
- Verify CPT and ICD-10 code compatibility before claim submission
- Follow payer-specific coverage policies and LCD guidelines
- Use coding validation tools and payer-edit software
- Train coding staff to review diagnosis-procedure pairings carefully
2. CO-18: Duplicate Claim or Service
Denial code CO-18 is issued when a payer identifies a claim as a duplicate of one that has already been submitted or processed. This can happen even when the duplicate submission was unintentional.
Why CO-18 Denials Occur
- A claim is resubmitted before the original claim has finished processing
- The same service is billed more than once for the same date of service
- System or clearinghouse errors result in duplicate transmissions
- A corrected claim is sent without properly updating claim identifiers or modifiers
- Billing staff resubmit claims without first checking payer responses
These denials are common in practices where claim tracking and follow-up processes are inconsistent.
Example
Submitting the same office visit claim twice for the same patient and date of service, without changing the claim reference number, will result in a CO-18 denial because the payer has already processed the service.
How to Fix a CO-18 Denial
- Check the payer’s claim status to confirm whether the original claim was paid, denied, or still pending
- Review the remittance advice to verify whether the service was already adjudicated
- If the service was legitimately repeated, resubmit the claim using the appropriate modifier to indicate a repeat procedure
- If the duplicate was submitted in error, do not resubmit; instead, void or disregard the claim
When required, submit an appeal with documentation explaining why the repeated service was necessary
How to Prevent CO-18 Denials
- Always confirm claim status before resubmitting
- Allow adequate payer processing time before taking follow-up action
- Use clearinghouse reports to monitor submissions and acknowledgments
- Establish clear internal workflows for corrected and resubmitted claims
3. CO-27: Insurance or Coverage Expired
Denial code CO-27 occurs when a claim is submitted for a date of service during which the patient’s insurance coverage was inactive, terminated, or expired. The payer confirms that the policy was not valid on the service date.
Common Reasons for CO-27 Denials
- The patient’s insurance plan ended before the date of service due to job loss, non-payment, or a change in coverage
- Eligibility was not verified on the day of the visit
- Incorrect date of service was entered on the claim
- Outdated insurance information was used during claim submission
- Coverage was retroactively terminated and not updated in the system
This denial frequently occurs when patients assume their coverage is still active or fail to report recent insurance changes.
Example
Billing an office visit for a patient whose insurance policy expired on the last day of the previous month will result in a CO-27 denial because coverage was inactive on the date of service.
How to Fix a CO-27 Denial
- Confirm the patient’s coverage status directly with the payer
- Review eligibility records to determine whether coverage was active on the service date
- If coverage was active, submit proof such as eligibility verification confirmation and appeal the denial
- If coverage truly expired, notify the patient and bill them according to your self-pay policy
A quick eligibility review often clarifies whether the denial is valid or appealable.
How to Prevent CO-27 Denials
- Verify insurance eligibility on the day of service, not just at appointment scheduling
- Ask patients to confirm insurance changes at check-in, especially at the start of a new month or year
- Use real-time eligibility tools through your practice or clearinghouse system
- Update insurance records immediately when coverage changes are identified
4. CO-29: Timely Filing Limit Expired
Denial code CO-29 is issued when a claim is submitted after the payer’s allowed filing deadline. Each insurance company sets a specific time limit for claim submission, and claims sent after that window are automatically denied, even if all other claim details are correct.
Common Reasons for CO-29 Denials
- Claims were held internally for too long before submission
- Corrected or resubmitted claims were sent after the filing deadline
- Delays occurred due to credentialing or insurance verification issues
- Claims were initially submitted to the wrong payer and corrected too late
- Staff were unaware of payer-specific filing limits
Timely filing limits vary by payer and plan type, which makes this denial especially common when deadlines are not actively tracked.
Example
Submitting a claim 120 days after the date of service to a payer that allows only 90 days for timely filing will result in a CO-29 denial, even if the claim information is otherwise accurate.
How to Fix a CO-29 Denial
- Review the payer’s timely filing policy to confirm whether the deadline was missed
- Check if the delay was caused by payer error, retroactive eligibility, or coordination of benefits issues
- If applicable, submit an appeal with documentation supporting the reason for late submission
- If the filing limit was clearly exceeded, the denial may be final and not appealable
Some CO-29 denials can be overturned, but only when strong proof exists.
How to Prevent CO-29 Denials
- Submit claims as soon as possible, ideally within 30 days of the date of service
- Track payer-specific filing limits and keep them accessible to the billing team
- Monitor claims that are on hold for missing information or internal review
- Escalate delayed claims before filing deadlines are reached
5. CO-16: Claim Lacks Information or Has Invalid Information
Denial code CO-16 occurs when a claim is missing required information or contains invalid or incorrect data. Because the payer cannot process the claim as submitted, it must be corrected before payment can be issued.
Common Reasons for CO-16 Denials
- Missing patient information such as name, date of birth, or insurance ID
- Invalid or missing provider identifiers (NPI or tax ID)
- Incorrect or missing modifiers
- Invalid CPT and ICD-10 code combinations
- Incorrect place of service or service location details
- Missing or incomplete authorization or referral numbers
CO-16 is one of the most frequent denial codes because it applies to a wide range of claim data errors and can affect both electronic and paper claims.
Example
Submitting a claim without the rendering provider’s NPI or with an invalid modifier will result in a CO-16 denial because required claim information is missing or incorrect.
How to Fix a CO-16 Denial
- Review the payer’s remittance advice to identify what information is missing or invalid
- Verify all patient, provider, and service details against the medical record
- Correct the identified errors in the claim
- Resubmit the corrected claim promptly to avoid timely filing issues
If the denial reason is unclear, contacting the payer directly can help clarify what needs to be corrected.
How to Prevent CO-16 Denials
- Use a pre-billing checklist to confirm all required claim fields are complete
- Validate provider and payer identifiers regularly
- Review claims for modifier and code accuracy before submission
- Maintain consistent internal workflows for claim review and quality checks
Missing or incorrect claim details remain one of the most frequent reasons claims get denied, especially when basic validation checks are skipped.
6. CO-96: Non-Covered Charges
Denial code CO-96 occurs when a claim is submitted for a service that the patient’s insurance plan does not cover. The service may be excluded from the benefit plan or not considered payable under the payer’s coverage rules.
Common Reasons for CO-96 Denials
- The service is excluded from the patient’s benefit plan, such as cosmetic procedures or non-covered screenings
- Coverage was inactive or expired on the date of service
- The claim was submitted under the wrong insurance plan or payer
- Required prior authorization was not obtained
- The diagnosis code does not support coverage or medical necessity for the service
CO-96 denials are commonly seen in specialties such as behavioral health, dermatology, and durable medical equipment (DME) billing.
Example
Submitting a claim for a cosmetic skin procedure to a standard medical insurance plan will result in a CO-96 denial because the service is not covered under the patient’s benefits.
How to Fix a CO-96 Denial
- Review the patient’s benefit details to confirm whether the service is covered
- Verify that the correct insurance plan and payer information were used
- If the issue is diagnosis-related, update the diagnosis code and resubmit the claim
- If coverage truly does not apply, bill the patient according to your financial policy
For services that may qualify, submit supporting documentation to demonstrate medical necessity
How to Prevent CO-96 Denials
- Verify eligibility and benefits before the appointment to confirm coverage requirements
- Confirm authorization requirements for services that may need approval
- Ensure the correct payer and plan are selected before claim submission
- Inform patients in advance when services may not be covered and obtain appropriate acknowledgments
7. CO-167: Diagnosis Not Covered
Denial code CO-167 occurs when the diagnosis code submitted on a claim is not considered payable for the billed service under the payer’s coverage rules. The payer determines that the diagnosis does not meet medical necessity requirements for that procedure.
Common Reasons for CO-167 Denials
- The ICD-10 diagnosis code does not meet the payer’s medical necessity criteria for the CPT code
- A general or outdated diagnosis code was used instead of a more specific one
- The diagnosis does not clinically support the type of service billed
- Local Coverage Determinations (LCDs) or National Coverage Determinations (NCDs) were not met
- A screening diagnosis was used when a covered clinical diagnosis was required
CO-167 denials are frequently seen in laboratory testing, imaging services, durable medical equipment (DME), and preventive care.
Example
Submitting a claim for wound care services with a diagnosis of hypertension will result in a CO-167 denial because the diagnosis does not support coverage for the service.
How to Fix a CO-167 Denial
- Review the payer’s coverage policies to confirm which diagnoses are payable for the service
- Check the medical record for additional or more specific diagnoses that support medical necessity
- Correct the diagnosis code and resubmit the claim
- If appropriate, include documentation that supports the clinical need for the service
How to Prevent CO-167 Denials
- Verify diagnosis-to-procedure compatibility before claim submission
- Use payer-specific tools or coverage guidelines to confirm diagnosis requirements
- Avoid using unspecified diagnosis codes when more precise options are available
- Inform patients in advance when a service may not be covered and obtain appropriate notices
8. CO-197: Precertification / Authorization Absent
Denial code CO-197 occurs when a service that requires prior authorization was performed without approval from the insurance payer. Because authorization was not obtained in advance, the payer denies payment for the claim.
Common Reasons for CO-197 Denials
- Prior authorization was required but not requested before the service
- Authorization was approved but linked to the wrong provider, facility, or date of service
- Authorization was requested too late or denied, but the service was still performed
- Approved visit limits were exceeded for recurring services
- Emergency services were billed incorrectly as non-emergent care
CO-197 denials are especially common for services such as advanced imaging, surgical procedures, therapy services, behavioral health care, and durable medical equipment (DME).
Example
Submitting a claim for an MRI without obtaining prior authorization from the payer will result in a CO-197 denial because approval was required before the service was performed.
How to Fix a CO-197 Denial
- Confirm whether prior authorization was required for the billed service
- Review authorization records to verify if approval was obtained but not properly documented
- If the service was medically necessary or provided in an emergency, submit an appeal with supporting clinical documentation
- If authorization was not obtained and no exception applies, the denial may not be appealable
How to Prevent CO-197 Denials
- Verify authorization requirements before scheduling procedures or services
- Maintain payer-specific authorization rules for commonly billed services
- Document authorization numbers clearly in the patient chart and billing system
- Track approved visit limits for recurring services and request extensions when needed
9. CO-204: Service Not Covered Under the Patient’s Current Benefit Plan
Denial code CO-204 occurs when a service is billed that is not included in the patient’s current insurance benefits. Even if the service was medically necessary, the payer will deny the claim if the plan does not cover that specific treatment.
Common Reasons for CO-204 Denials
- The service is excluded under the patient’s benefit plan, such as certain cosmetic or elective procedures
- Coverage is limited to specific conditions that were not met
- The claim was submitted under an incorrect or outdated insurance plan
- The wrong plan option was selected during eligibility verification
- Confusion between in-network and out-of-network coverage
CO-204 denials are especially common when benefit details are not fully reviewed before services are provided.
Example
Submitting a claim for a therapy service that is excluded under the patient’s insurance plan will result in a CO-204 denial because the service is not covered by the current benefit plan.
How to Fix a CO-204 Denial
- Review the patient’s benefit details to confirm whether the service is covered
- Verify that the correct insurance plan and coverage option were billed
- If the wrong plan was used, correct the insurance information and resubmit the claim
- If the service is truly non-covered, inform the patient and follow your self-pay or payment plan process
For borderline cases, submit clinical documentation requesting reconsideration when appropriate
How to Prevent CO-204 Denials
- Verify benefits thoroughly before providing services
- Review payer-specific coverage rules and exclusions in advance
- Confirm in-network and out-of-network coverage details
- Communicate clearly with patients when services may not be covered
10. CO-B7: Provider Not Credentialed with the Payer
Denial code CO-B7 occurs when a claim is submitted under a provider who is not credentialed or enrolled with the insurance payer for the billed service. Because the provider is not recognized by the plan, the payer denies the claim.
Common Reasons for CO-B7 Denials
- A new provider began seeing patients before credentialing was completed
- Claims were submitted before the credentialing effective date
- An incorrect billing or rendering NPI was used on the claim
- The provider is credentialed with the payer but not with the specific plan or network
- Credentialing applications were delayed, incomplete, or still under review
CO-B7 denials are especially common with Medicaid managed care organizations, Medicare Advantage plans, and commercial payers with limited provider networks.
Example
Submitting a claim for services rendered by a newly hired provider before their credentialing approval date will result in a CO-B7 denial because the provider is not yet enrolled with the payer.
How to Fix a CO-B7 Denial
- Verify whether the provider has been fully credentialed and the effective date of approval
- Confirm that the correct billing and rendering NPI numbers were used
- If the provider was credentialed at the time of service, submit proof of approval and resubmit the claim
- If credentialing was still in progress, hold or rebill claims according to the payer’s backdating rules
How to Prevent CO-B7 Denials
- Complete credentialing and payer enrollment before providers begin seeing patients
- Maintain a credentialing tracker with approval dates and recredentialing timelines
- Review NPI and taxonomy details regularly to ensure accuracy
- Coordinate closely between billing, credentialing, and administrative teams
11. CO-109: Claim Not Covered by This Payer / Contractor
Denial code CO-109 occurs when a claim is submitted to an insurance payer or contractor that is not responsible for payment. The payer denies the claim because another insurer should have been billed instead.
Common Reasons for CO-109 Denials
- The patient’s primary insurance changed, but the previous payer was billed
- The patient has multiple insurance plans and the incorrect payer was selected
- A claim was submitted to Medicare instead of a Medicare Advantage plan, or vice versa
- Incorrect payer ID or manual entry errors during claim submission
- Claims were routed to the wrong regional Medicare contractor
CO-109 denials are especially common when patients change jobs, insurance plans, or coverage mid-year.
Example
Submitting a claim to Medicare for a patient enrolled in a Medicare Advantage plan will result in a CO-109 denial because the claim was sent to the wrong payer.
How to Fix a CO-109 Denial
- Verify the patient’s current primary and secondary insurance coverage
- Review eligibility information to confirm the correct payer and plan
- Update the claim with the correct payer details
- Resubmit the claim to the appropriate insurance carrier
How to Prevent CO-109 Denials
- Confirm active insurance and payer responsibility at every patient visit
- Ask patients about recent insurance changes or additional coverage
- Use real-time eligibility verification tools to validate payer information
- Pay close attention to Medicare replacement and Advantage plan enrollment
12. CO-50: Non-Medically Necessary Service
Denial code CO-50 occurs when a payer determines that a billed service was not medically necessary based on the diagnosis, clinical documentation, or the payer’s medical necessity policies.
Common Reasons for CO-50 Denials
- The diagnosis code does not support the medical necessity of the procedure
- The service is considered routine, preventive, or cosmetic under the payer’s policy
- Clinical documentation is insufficient or lacks detail to justify the service
- National or Local Coverage Determinations (NCDs/LCDs) were not met
Prior authorization was required to establish medical necessity, but was not obtained
CO-50 denials are commonly seen in dermatology, pain management, behavioral health, and outpatient surgical services.
Example
Submitting a claim for an advanced diagnostic test without documentation explaining why the test was medically necessary will result in a CO-50 denial.
How to Fix a CO-50 Denial
- Review the payer’s medical necessity guidelines for the billed service
- Ensure the diagnosis code accurately reflects the patient’s condition
- Submit an appeal with detailed clinical notes, test results, or physician statements
- Include any relevant authorization or supporting documentation if available
How to Prevent CO-50 Denials
- Confirm that ICD-10 diagnosis codes clearly support the billed CPT codes
- Follow payer-specific NCD and LCD guidelines for high-risk services
- Maintain detailed and specific clinical documentation
- Use modifiers such as GA or GZ appropriately when Advance Beneficiary Notices (ABNs) apply
Conclusion
Medical billing denials are common, but most can be avoided with accurate coding, strong documentation, and consistent front-end verification. Understanding why denials occur and addressing them early helps reduce rework, prevent payment delays, and protect revenue.
For practices that prefer to offload this workload, outsourcing to experts offering denial management services can help reduce denials, speed up reimbursements, and improve overall revenue performance.
Frequently Asked Questions
Find quick answers to common questions about this topic, explained simply and clearly.
What is the most common claim denial?
Eligibility or coverage not active on the date of service. Other frequent causes: missing prior authorization, invalid member ID, and timely filing exceeded.
What are denial codes in medical billing?
Standard code sets on remits that explain why a claim or line was reduced or denied. Two types: CARC (Claim Adjustment Reason Codes) and RARC (Remittance Advice Remark Codes).
What is 97 denial?
CARC 97 - Payment is included in the allowance for another service or procedure (bundled/duplicate per plan rules).
What does denial code 222 mean?
CARC 222 - Exceeds the plan or contract limit for the number of services/units in the allowed time period.
What is CO 27 denial?
CO-27 - Expenses incurred after coverage terminated (patient not covered for the service date).