CPID In Medical Billing - Explained For Billing Teams
- Updated Date Oct 23, 2025
- Medical Billing
- Follow
Ever had a batch of clean claims bounce for no clear reason? Many times, the issue is not the diagnosis or the CPT. It is the CPID. CPID is the payor ID used by clearinghouses to steer your claim. It can change by plan, state, or claim form. Using the wrong one slows cash and frustrates staff. Here you will learn what CPID really is, where to find it, and how to pick the right ID for CMS 1500 and UB-04.
What CPID Means in Medical Billing?
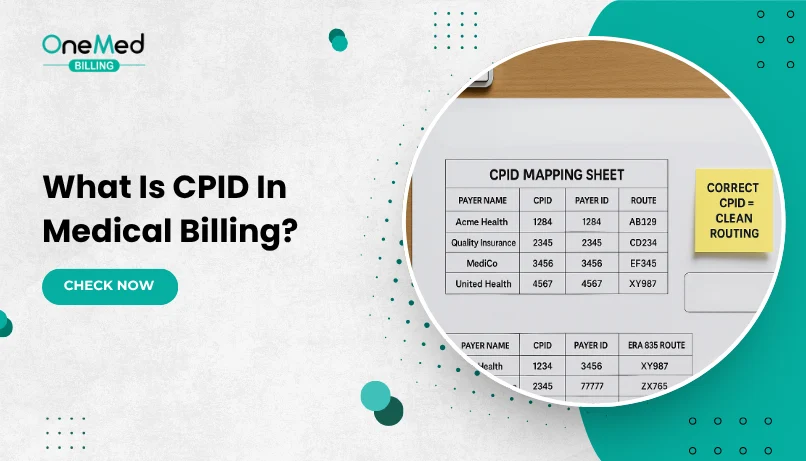
CPID stands for Claims Payer ID. It is the code your clearinghouse uses to route a claim to the exact payor and plan. Think of it like the street address on an envelope. If the address is precise, the claim reaches the right place and gets processed. If it is off, the claim bounces back, and you lose time.
Here is the part many teams miss. A CPID is not always the same as a generic payor ID. It can vary by clearinghouse, by plan, by state, and even by claim type. The CPID that works for a professional claim may not work for an institutional claim. The number printed on a member card might help, but the safest source is the payor list inside your
clearinghouse.
Where to Find the Right CPID for Your Claim?
You will find the correct CPID inside your clearinghouse. That is the most reliable source. Follow these simple steps.
Step by step
- Sign in to your clearinghouse portal.
- Open Payor List or Payor Search.
- Type the payor name and choose the exact plan or line of business.
- Check for state notes. Some plans use different IDs by state.
- Select the claim type you are sending. Professional for CMS 1500. Institutional for UB 04.
- Copy the CPID exactly as shown. Do not change spacing or digits.
- Read any notes on attachments, secondary routing, or paper claims.
- Add the CPID to your practice management or EHR payor setup.
- If you bill both professional and institutional, add each CPID to the correct place.
- Save your changes and keep a short note of when and who updated it.
Other places to confirm
- Your EHR or billing software may show a payor ID table that mirrors the clearinghouse list.
- The number on the member card can help, but always verify against the clearinghouse list before sending claims.
- If you changed clearinghouses, ask for a CPID crosswalk so you can map old IDs to new ones.
CPID vs Payer ID vs EDI Payer ID
These terms sound alike, but they are not always the same. Here is the simple way to tell them apart and pick the right one.
Plain meanings
- CPID means Claims Payer ID. It is the routing code your clearinghouse uses to send a claim to the exact payor and plan. It can differ by clearinghouse and by claim type.
- Payer ID is a general label for the number a payor publishes. Sometimes it matches your clearinghouse’s CPID. Sometimes it does not.
- EDI Payer ID is the identifier used inside the electronic claim file. Your software maps this to the correct payor based on the clearinghouse’s setup.
Quick comparison
| Term | What it does | Who sets it | Can it vary by clearinghouse | Can it vary by claim type | Where to verify |
|
CPID |
Routes the claim inside your clearinghouse | Clearinghouse | Yes | Yes, pro vs inst | Clearinghouse payer list |
|
Payer ID |
Generic payer identifier, may appear on cards or sites | Payer, sometimes shared widely | Sometimes | Sometimes | Still confirm in the clearinghouse list |
|
EDI Payer ID |
The ID used in the 837 file to identify the payer | Your software and clearinghouse mapping | Follows the mapping | Follows the mapping | Your software’s payer setup and clearinghouse list |
How to decide which one to use?
1. Start with your clearinghouse payor list. Select the exact plan and claim type.
2. Use the CPID shown there. That is the safest value for routing.
3. If a payor ID from a card or website differs, trust the clearinghouse list.
4. Make sure your software’s payor record maps the EDI payor ID to the same entry.
What to Watch When Setting Up CPID?
Setting up CPID looks simple, but it decides where your claim lands. Get it right, and routing is clean with fewer rejections. Get it wrong and you add phone calls, rework, and slow cash. Before you lock in an ID, pause for a quick review of the details that most often cause problems. The points below walk you through what to check so your claims move on the first try.
1. Pick the exact plan and claim type
Choose the specific plan and select professional for CMS 1500 or institutional for UB 04. Do not reuse one ID for both. If you bill both forms, save both IDs and label them clearly so staff pick the right one.
2. Confirm state and line of business
Check state notes and whether the plan is Commercial, Medicaid, Medicare Advantage, or Exchange. IDs can change by line of business. Match the plan on the card to the exact entry in your clearinghouse list.
3. Use the clearinghouse payor list
Treat the payor list in your clearinghouse as the source of truth. Card numbers and websites can differ. Search by payor name, pick the exact plan, and read any notes about limits or attachments.
4. Map the ID in your software
Paste the CPID into the correct payor record and label it clearly. Keep separate entries for professional and institutional if needed. Limit edits to admins and add an effective date so you know when it changed.
5. Test before you send volume
Run one eligibility check or a single low risk claim. Confirm that routing returns clean. If it fails, recheck the plan, state, and claim type before you send more.
6. Keep a simple crosswalk
Maintain a small sheet with payor, plan, state, professional CPID, institutional CPID, notes, and last verified date. Update it monthly. Share it in a read only location and highlight any changes to top payors.
7. Watch for special cases
Look for paper claim CPIDs, attachment rules, secondary claim routing, and payor rebrands after mergers. Some Medicaid and Medicare Advantage plans use unique entries. Secondary claims may need a different route.
8. Train your team
Show staff how to look up CPIDs and when to recheck them. Add a quick checklist to onboarding. Include simple screenshots from your own system and refresh training after a clearinghouse switch.
9. Document changes
Record who updated the ID, when it changed, and why. This helps you trace issues fast if rejections spike. Keep a short audit note or ticket link inside the payor record.
How CPIDs Vary by Clearinghouse and Claim Type?
CPID is not a single national code. Different medical billing clearing houses keep their own routing tables, so the same payor can have a different CPID from one clearinghouse to another. Many payors also use one CPID for professional claims (CMS 1500) and another for institutional claims (UB 04). Plan, state, and line of business can change the ID again.
Why this happens
- Clearinghouses use their own networks and assign IDs that fit their routing.
- Payers split products by line of business or by state, so one brand can have multiple entries.
- Professional and institutional claims follow different processing paths, so they often need separate IDs.
What to do
- Always select the exact plan and claim type in your clearinghouse payor list.
- Check for state notes and line of business labels before you copy the ID.
- Save both IDs if you send both professional and institutional claims.
How To Verify a CPID in Two Minutes?
Run a quick check before you send a batch. Open your clearinghouse, go to the payor list, and search for the payor. Choose the exact plan or line of business, pick the claim type you will send (professional for CMS 1500, institutional for UB 04), review any state or product notes, and copy the CPID exactly as shown.
Next, open your billing software and paste the CPID into the payor record for that plan and claim type. Save your changes so the mapping is in place for the claim you are about to send.
Now send a small test, such as an eligibility check or one low risk claim. Confirm that the routing returns clean. If it fails, recheck the plan and line of business, make sure the claim type matches the CPID you selected, and look for a state specific entry for the same payor.
To keep things tidy, maintain a simple CPID log with payor, plan, state, professional CPID, institutional CPID, notes, and last verified date. Update it when you switch clearinghouses or when a payor changes products or routing.
Choose the Right CPID for CMS 1500 and UB-04
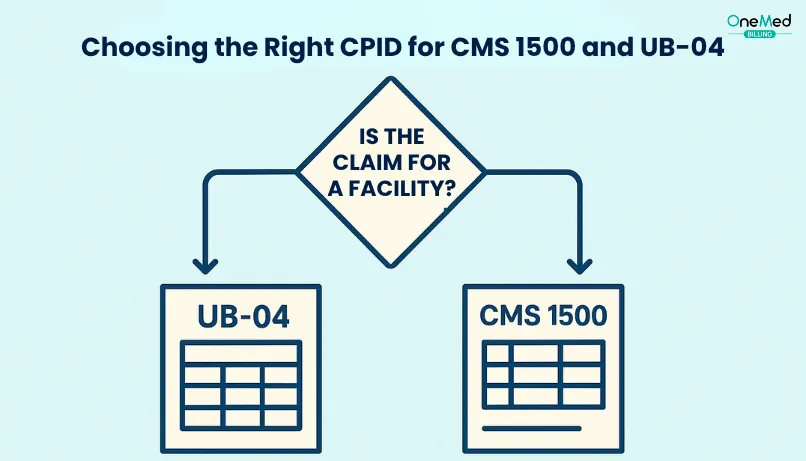
CMS 1500 is for professional claims. UB 04 is for institutional claims. Many payors use a different CPID for each, so reusing one ID across both forms can cause rejections.
In your clearinghouse, open the payor list, pick the exact plan and line of business, choose the claim type you are sending, and copy the CPID exactly as shown. Save it in your billing software under the matching claim type.
Send a quick test, an eligibility check, or one low risk claim. If you see a routing error, recheck the plan, state, and claim type. Some payors also list a separate CPID for paper claims. Use that only when you mail CMS 1500 or UB-04.
Conclusion
Getting CPID right pays off. When the ID matches the plan, state, and claim type, first pass yield goes up, denials drop, and days in A/R come down. Your staff spends less time on phone calls and resubmits, and more time on patient-facing work.
Keep it simple. Use the clearinghouse payor list as your source of truth, save separate IDs for CMS 1500 and UB 04, run one quick test before volume, and keep a small crosswalk that you review each month. Recheck CPIDs after payor rebrands, plan mergers, or a clearinghouse change.
Frequently Asked Questions
Find quick answers to common questions about this topic, explained simply and clearly.
What is a CPID?
A CPID is the Claims Payer ID your clearinghouse uses to route a claim to the exact plan.
What are common uses for a CPID?
Routing electronic claims, mapping payers in your software, and separating professional and institutional submissions.
What is the difference between payer ID and CPID?
Payer ID is the insurer’s identifier. CPID is the clearinghouse routing ID. Always confirm the CPID in your clearinghouse.
What are some CPID examples?
Formats vary. Example only Professional CPID 1245, Institutional CPID 6789 for the same plan. Always verify in your clearinghouse.