Precertification vs Preauthorization - Similar But Not The Same
- Updated Date January 17th, 2026
- Prior Authorization
- Follow
Precertification and preauthorization are two terms that often confuse providers. Both involve getting approval from an insurance company before a service is given, but they are not always used in the same way. This guide explains what each means, how they differ, and why understanding the distinction is important for providers.
What Is Preauthorization?
Preauthorization means getting approval from a patient’s insurance company before certain services or treatments can be provided. In most cases, it isn’t the doctor personally who requests it, but rather the provider’s staff, front desk, or billing team who handle the paperwork. It’s not required for every service, and it’s not limited only to high-cost care; sometimes even routine or lower-cost treatments may need preauthorization, depending on the insurance plan.
In practice, the provider sends medical details to the payor, which might include the doctor’s notes, diagnosis codes, test results, or a history of past treatments. Most requests are submitted through an online portal, though some payors still accept fax submissions. The payor reviews the request against its medical necessity guidelines. If approved, the service can move forward and be billed to insurance. If a claim is denied or delayed, providers must reappeal, leading to longer wait times for patients and potential out-of-pocket costs if the appeal is unsuccessful.
What Is Pre-Certification?

Precertification means a provider must check with the patient’s insurance company before admitting them to a hospital or scheduling certain procedures. In simple terms, it is the payor’s way of confirming that the planned care is medically necessary and will be covered.
In real-world settings, precertification is most often required for inpatient hospital stays, surgeries performed in a facility, or admissions to rehab, skilled nursing, or long-term care centers. If approval is not obtained in advance, the insurance company may refuse payment, requiring providers to reappeal claims and causing patients to wait longer for resolution.
To complete this step, the provider’s office usually submits information such as the admitting doctor’s notes, diagnosis codes, or recent test results. Most payors prefer submissions through their online portal, although some still accept fax. Once received, the payor reviews the request and gives a decision. An approval allows the patient to move forward with treatment, while a denial or delay may require more documentation or an appeal.
Difference Between Precertification and Preauthorization
Preauthorization and precertification are terms that people often mix up, and while they do share some similarities in various insurance policies, there are key differences between the two.
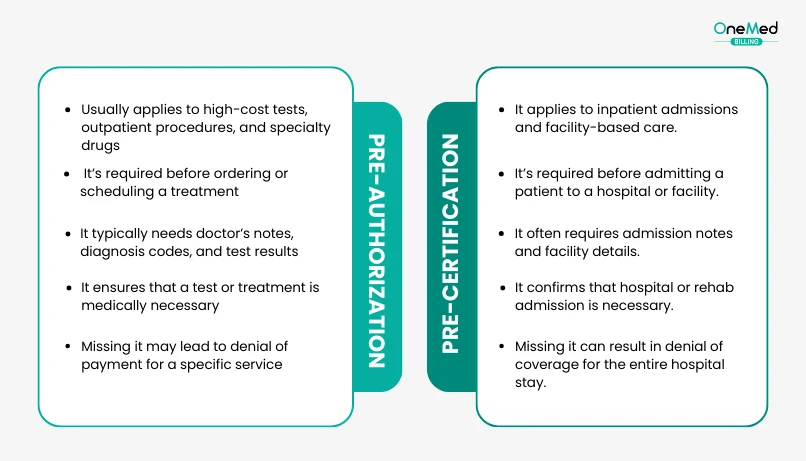
1. Type of Service
Preauthorization usually applies to high-cost tests, outpatient procedures, or specialty drugs. Precertification is more commonly required for inpatient hospital stays, surgeries at a facility, or admissions to rehab and skilled nursing.
2. Timing
Preauthorization is generally requested before a test, treatment, or medication is ordered. Precertification, on the other hand, is required before a patient is admitted to a hospital or booked into a facility.
3. Documentation
Both need clinical details, but precertification often requires extra information, such as admission notes and facility details, in addition to diagnosis and test results.
4. Consequences of Skipping
Missing either step can lead to a denied claim. With precertification, this often means that coverage for the entire hospital stay may be refused.
5. Patient Impact
A missed preauthorization can delay important scans or specialty medications, leaving patients waiting longer than expected. A missed precertification can go even further, causing a scheduled surgery or hospital admission to be cancelled at the last minute.
6. Financial Risk
Missing preauthorization may lead to the denial of a $2,000 test or medication. Missing precertification is riskier, as it could mean denial of an entire $20,000 - $30,000 hospital admission, creating major financial stress for both patients and providers.
Conclusion
Preauthorization and precertification often sound alike, but in practice, they cover different things. Preauthorization is usually needed for tests, treatments, or costly drugs, while precertification is mostly tied to hospital admissions and facility-based care. Both steps exist because insurance companies want to confirm the care is necessary before they agree to pay.
If a provider skips either one, claims can be denied, and patients may face delays or surprise bills. That’s why it helps to know the difference and have a clear process in place. Some practices choose to outsource prior authorization to specialized billing partners to keep the work from piling up.
At the end of the day, understanding preauthorization and precertification helps everyone involved; patients are less likely to be hit with unexpected costs, and providers can deliver care with fewer payment delays or financial setbacks.
Frequently Asked Questions
Find quick answers to common questions about this topic, explained simply and clearly.
Are precertification and preauthorization the same thing?
Not always. Some insurance companies use the terms interchangeably, but others treat them differently. Preauthorization usually applies to tests, drugs, or outpatient care, while precertification is often for hospital admissions or surgeries.
What is the purpose of precertification?
The purpose of precertification is to make sure that a planned hospital stay, surgery, or facility-based service is medically necessary and covered by insurance. It protects patients from surprise costs and helps providers avoid claim denials.
Who is responsible for getting preauthorization or precertification?
Usually, the provider’s office or hospital staff submits the request, but patients should confirm with their doctor’s office to avoid delays or denials.
How long is a pre-authorization valid?
The validity of a pre-authorization depends on the insurance company. In most cases, approvals last between 30 to 90 days. If the service is not provided within that time, a new request may be required.