5 Types of Authorization in Medical Billing and Why They Matter
- Updated Date January 17th, 2026
- Medical Billing
- Follow
Authorization in medical billing is the approval a provider must obtain from an insurance company before delivering certain treatments, procedures, or medications. It ensures that the service is covered, medically necessary, and in line with payor rules.
For providers, authorization helps prevent claim denials; for payors, it controls costs; and for patients, it reduces the risk of unexpected bills. In this blog, you will learn about the main types of authorization in medical billing and why each one is important.
Types of Authorization in Medical Billing
Authorization is not the same in every situation, and different types are required depending on the service being provided. Below are the main types of authorization in medical billing that providers use to secure approval and ensure proper reimbursement.
1. Prior Authorization (also known as Preauthorization or Precertification)
Prior authorization is approval from a payor before a medical service, procedure, medication, or hospital admission takes place. Insurance companies use this process to confirm that the treatment is medically necessary and follows coverage guidelines. In many insurance plans, this same process may be labeled differently, which is why understanding of how preauthorization and precertification differ can be helpful.
Providers typically submit diagnosis codes, procedure codes, and supporting medical records to justify the request. This may include clinical notes, test results, or previous treatment history.
Prior authorization is commonly required for high-cost drugs, advanced imaging such as MRIs and CT scans, inpatient admissions, and complex surgeries. Approved authorizations often come with limits, such as a specific number of visits, time frames, or dosage amounts. Missing or incorrect documentation is a common reason for delays and denials. For a more detailed overview of the process, in-depth knowledge of prior authorization is covered in a separate guide.
Additional key points:
- Authorizations usually have an expiration date and must be used within a specific time period
- Some approvals are provider- or facility-specific
- Changes to the treatment plan may require a new authorization
- Appeals can often be filed if a request is denied
2. Concurrent Authorization
Concurrent authorization is used when a patient is already receiving care and continued approval is needed for ongoing treatment. This is most common in inpatient hospital stays, rehabilitation centers, and long-term therapy services.
During treatment, providers must send progress updates and clinical documentation to the insurance company. The insurer reviews this information to decide whether continued care remains medically necessary.
For example, if a patient remains hospitalized longer than originally expected, the provider must request approval for additional days. Without concurrent authorization, insurers may refuse payment for extended services.
Additional key points:
- Reviews often happen every few days or weekly during inpatient stays
- Insurers may approve only a limited number of days at a time
- Delayed documentation can interrupt coverage
- Care managers frequently assist with this process
3. Retroactive Authorization
Retroactive authorization is requested after services have already been provided. This usually applies to emergency or urgent situations where waiting for approval is not possible.
Examples include trauma care, emergency surgeries, and sudden hospital admissions. After treatment, providers submit documentation explaining the medical urgency and necessity of the service.
Because insurers prefer authorization before care, retroactive requests carry a higher risk of denial. Strong clinical documentation is essential to improve the chances of approval.
Additional key points:
- Often requires proof that the situation was truly emergent
- Time limits may exist for submitting requests
- Denials are more common than with prior authorization
- Appeals are frequently needed for payment approval
4. Referral Authorization
Referral authorization is required when a patient’s primary care physician sends them to a specialist, especially in managed care plans such as HMOs.
The authorization confirms that the specialist visit is covered under the patient’s insurance plan and often includes limits on the number of visits or time allowed.
For instance, a patient referred to a cardiologist for heart-related concerns may need referral authorization before the appointment. Without it, the insurance company may deny payment for the specialist services.
Additional key points:
- Referrals are usually valid only for specific specialists
- Many plans restrict the number of approved visits
- Expired referrals require renewal
- Self-referrals often result in denied claims
5. Ongoing or Extended Care Authorization
Some treatments require authorization in phases rather than a single approval. This is common for services that continue over time.
Examples include physical therapy, mental health counseling, home health services, and durable medical equipment. Insurance companies may approve a set number of visits or a defined treatment period.
If additional care is needed, providers must submit progress reports and request further authorization. Continued coverage depends on showing that the treatment remains medically necessary.
Additional key points:
- Progress notes are required for extensions
- Insurers may reassess patient improvement
- Treatment caps may apply
- Lack of follow-up can stop coverage
Common Services That Require Authorization
Many insurance plans require authorization for services that are high-cost, complex, or long-term. While requirements vary by payor, the following services commonly need approval before they are provided.
Advanced imaging tests such as MRIs, CT scans, and PET scans almost always require authorization. These tests are expensive and insurers use the process to confirm medical necessity before approving payment.
Surgeries and invasive procedures often need authorization, especially elective or non-emergency operations. This includes orthopedic surgeries, cardiac procedures, and many outpatient surgical services.
Specialty and high-cost medications frequently require approval, particularly biologics, cancer treatments, and injectable drugs. Insurers review these requests to ensure the medication is appropriate and follows treatment guidelines.
Inpatient hospital admissions usually require authorization or precertification before the patient is admitted, unless it is an emergency. Continued stays often require concurrent authorization as well.
Physical therapy and rehabilitation services commonly need approval for a set number of visits. If more sessions are required, providers must request additional authorization to continue care.
Because each insurance plan sets its own rules, it is always important to verify authorization requirements before scheduling services.
Who Is Responsible for Getting Authorization?
Although providers lead the authorization process, it involves collaboration across multiple roles.
- Physicians and clinical teams supply medical justification and treatment details
- Authorization or billing staff communicate with insurers and monitor approvals
- Patients may help verify benefits or respond to insurer requests
Importance of Authorization in Medical Billing

Authorization is a critical part of the billing process because it safeguards providers, payors, and patients. Its importance can be explained in several ways:
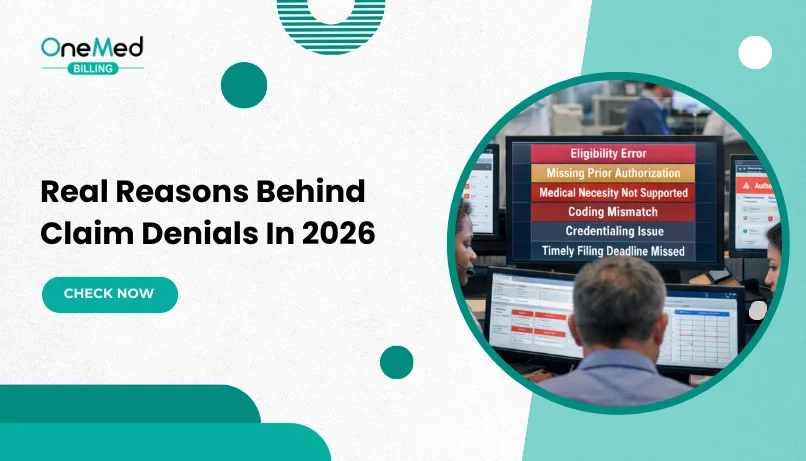
- Prevents claim denials by getting approval in advance and reducing the most common reason for rejected claims. This saves staff time, minimizes rework, and keeps the revenue cycle moving smoothly.
- Ensures compliance with payor rules since every insurer has specific requirements for which services need authorization. Following these rules helps providers avoid audits, penalties, and disputes.
- Protects providers from financial loss because services without authorization may go unpaid. By confirming coverage upfront, providers avoid absorbing costs or passing them to patients.
- Improves patient transparency by giving patients a clearer idea of what is covered and what may fall under out-of-pocket costs. This reduces confusion and builds trust in the billing process.
The Role of Technology in Authorization Management
Technology has become an essential tool in managing authorizations within the medical billing process. Modern billing software and electronic health record (EHR) systems now include features that automatically check payor requirements, submit authorization requests, and track their status in real time. This reduces manual errors, saves staff time, and helps ensure that approvals are obtained before services are performed.
Automated systems also provide alerts for pending or expiring authorizations, giving staff the chance to act before a claim is denied. By integrating technology into authorization workflows, providers can streamline communication with payors, reduce delays in patient care, and protect revenue from unnecessary losses.
Best Practices to Speed Up Authorization Approvals
Providers can reduce delays and speed up authorization approvals by following a few proven practices:
- Train staff regularly on payor-specific requirements so they know exactly what documentation to submit.
- Use billing software or EHR systems with built-in authorization tracking and alerts to prevent missed deadlines.
- Maintain complete and accurate patient records to avoid back-and-forth requests for additional details.
- Establish clear communication channels with payors for faster responses and fewer disputes.
- Consider outsourcing prior authorization tasks to specialized teams that can manage the process more efficiently.
Conclusion
Authorization in medical billing comes in different forms, including prior authorization, preauthorization, concurrent authorization, retroactive authorization, and referral authorization. Each type serves a specific purpose in ensuring services are covered, medically necessary, and aligned with payor rules.
Handling authorizations correctly is essential for smooth revenue cycle management. It helps providers avoid denials, protect revenue, and maintain compliance, while also giving patients more clarity about their coverage. By staying proactive and organized, healthcare organizations can turn the authorization process into a safeguard rather than a barrier.
Frequently Asked Questions
Find quick answers to common questions about this topic, explained simply and clearly.
What is an authorization in medical billing?
Authorization in medical billing is advanced approval from an insurance company that confirms a treatment, procedure, or medication is covered and medically necessary.
What is pre-authorization and post-authorization?
Pre-authorization is approval obtained before a service is performed, while post-authorization (retroactive) is requested after the service, usually in urgent or emergency cases.
What is a reverse authorization?
Reverse authorization happens when a previously approved service is canceled or reversed, often due to changes in the patient’s treatment plan or insurance coverage.
What happens if a service is done without authorization?
The claim may be denied, leaving providers unpaid and patients responsible for the cost.