How Long Does It Take to Get a Prior Authorization in 2026?
- Updated Date Feb 5, 2026
- Prior Authorization
- Follow
According to the Centers for Medicare & Medicaid Services (CMS), expedited prior authorization requests must be reviewed within 72 hours, while standard requests are typically processed within 7 calendar days for Medicare Advantage plans. Major commercial insurers such as UnitedHealthcare, Aetna, and Blue Cross Blue Shield generally complete routine authorizations within 5 to 10 business days. UnitedHealthcare’s own provider guidelines explain that standard prior authorization decisions may be rendered within approximately three to ten business days, depending on the completeness of supporting documentation and any additional medical review needed. With complex cases like specialty medications or surgical approvals extending up to 14 to 21 days, depending on clinical review requirements.
Despite these defined timelines, many approvals still stretch longer due to documentation gaps, medical policy reviews, and workflow delays.give me the links to the soruces
What is Prior Authorization?
Prior authorization is when a healthcare provider gets approval from a patient’s insurance company before giving certain treatments, tests, or medications. This step is meant to confirm that the service is medically necessary and will be covered under the patient’s plan.
The time it takes to get a prior authorization can make a big difference for both patients and providers. For patients, delays can mean waiting longer to start important treatments or receive needed medications. For providers, these delays can disrupt the care schedule, create extra paperwork, and even affect payment timelines. Understanding the prior authorization process is key to avoiding unnecessary holdups and working toward faster prior authorization approval.
When handled efficiently, prior authorization helps ensure that treatments are approved before they start, reducing the risk of unexpected bills and helping providers keep the care process smooth from start to finish. However, when requests get stuck or insurance companies take too long to respond, it can lead to frustration, missed appointments, and even common medical billing denials later on.
Prior Authorization Timelines by Major Insurance Providers
While prior authorization timelines can vary based on the type of service, urgency, and documentation quality, most major insurance companies follow general processing windows. Understanding these average timeframes helps providers plan patient care more efficiently and avoid unnecessary delays.
Below are real-world averages commonly experienced by healthcare practices:
1. Aetna Prior Authorization Timeline
Aetna typically processes standard prior authorization requests within 3 to 5 business days when submitted through their electronic provider portal or via approved clearinghouses.
Factors that may speed up approval:
- Complete clinical documentation
- Correct CPT and ICD-10 codes
- Electronic submission (faster than fax)
Common delay causes:
- Missing progress notes or imaging reports
- Medical necessity not clearly stated
Urgent requests are often reviewed within 24-72 hours if marked correctly.
2. Blue Cross Blue Shield (BCBS) Timeline
BCBS timelines vary slightly by state plan, but most standard requests are completed within 2 to 7 business days.
Faster approvals occur when:
- Requests are submitted through BCBS online portals
- Policy-specific guidelines are followed
- Supporting documents are uploaded correctly
Delays often happen due to:
- Incorrect plan selection
- Incomplete authorization forms
- Service not meeting medical policy criteria
Urgent reviews may be completed within 24-48 hours.
3. UnitedHealthcare Timeline
UnitedHealthcare typically reviews standard prior authorization requests within 3 to 10 business days, depending on service complexity and documentation quality.
Best practices for faster turnaround:
- Use the UnitedHealthcare Provider Portal
- Attach all clinical evidence upfront
- Double-check benefit eligibility before submission
Faster approvals occur when:
- High-cost imaging or specialty procedures
- Requests requiring medical director review
- Clarification requests from the payer
Expedited requests are usually resolved within 72 hours.
4. Medicare Prior Authorization Timeline
Medicare follows strict regulatory timelines:
Urgent requests: typically 1-3 business days
Standard requests: usually 3-7 business days
Approvals depend heavily on:
- Clear proof of medical necessity
- Compliance with Medicare coverage rules
- Accurate coding and documentation
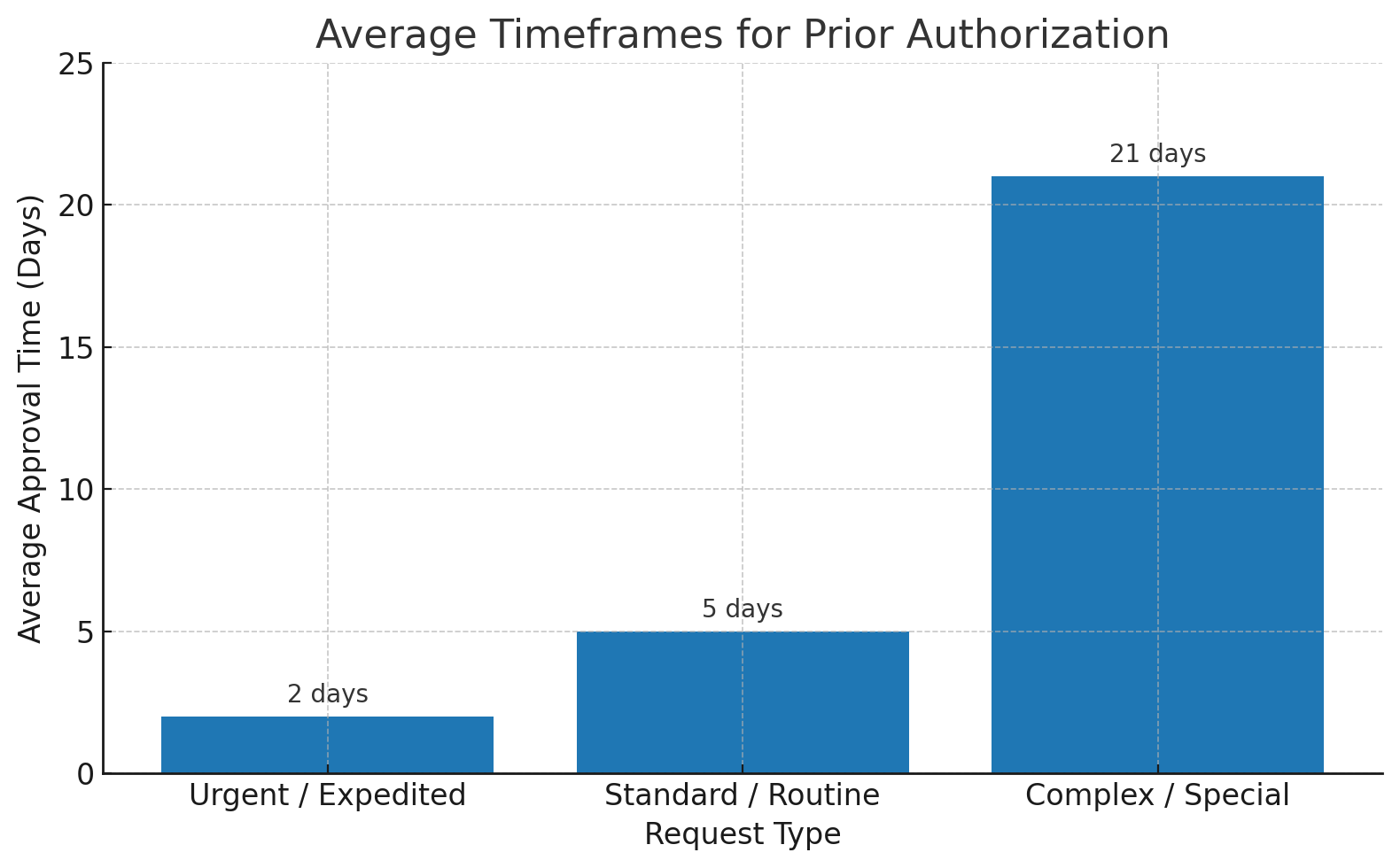
Average Timeframes for Prior Authorization
The time it takes to get a prior authorization depends on how urgent the request is, the type of service, and the insurance company’s process. Knowing these timeframes can help both patients and providers plan ahead and avoid last-minute delays.
1. Urgent or Expedited Requests
If a patient’s health could seriously worsen without immediate treatment, the provider can request an urgent or expedited review. In most cases, insurance companies aim to respond within 24 to 72 hours. Approvals are often faster when the request is well-documented and the insurance eligibility check is done correctly. Using the best practices for verifying insurance eligibility ensures all details are accurate before submission, which can make a big difference in urgent cases.
2. Standard or Routine Requests
For most medical services and non-urgent treatments, the approval process takes longer. On average, 3 to 7 business days is common. This timeframe applies to regular diagnostic tests, outpatient procedures, and non-emergency prescriptions. Providers who plan ahead submit requests early, monitor their progress closely, and stay in regular contact with the payer to keep the approval process on track.
3. Complex or Special Cases
Some requests are more complicated and can take several weeks to approve. These often involve high-cost treatments, specialized medications, or procedures that require multiple layers of review. Complex requests may also need supporting documentation from more than one provider or specialist. Understanding the provider credentialing process and knowing the payer’s specific requirements can help speed up these cases and work toward faster prior authorization approval.
Factors That Affect Prior Authorization Timelines
The time it takes to get a prior authorization approved can be different for every patient and request. Even similar treatments may move faster or slower based on a few key factors. Knowing what affects the timeline helps healthcare providers avoid delays and get approvals quicker.
1. Type of Service, Treatment, or Medication
Simple and common services usually get approved faster. These include routine tests, basic imaging, or standard medications.
More complex or expensive treatments often take longer. This may include surgeries, specialty drugs, advanced scans, or new therapies. Insurance companies usually review these carefully to make sure they are medically necessary.
For example:
- A basic MRI may be approved in 1-3 days
- A specialty medication may take 7-14 days
Insurance companies may ask to see proof that lower-cost treatments were tried first.
Tip to speed things up: Clearly explain why the treatment is needed and include doctor notes with the request.
2. How Complete the Paperwork Is
Missing documents are the biggest reason for delays.
Insurance companies often pause requests when they don’t receive:
- medical notes
- test results
- correct billing codes
- treatment history
Even one missing file can slow the whole process.
For example, BCBS may delay imaging approvals without reports, and UnitedHealthcare often asks for extra clinical details.
Tip to speed things up: Always submit all required documents together the first time.
3. Insurance Company Rules and Review Process
Every insurance company works differently.
Some approve simple requests automatically. Others send complex cases to medical reviewers. Some respond faster to online submissions than fax or phone requests.
For example:
- Medicare often handles urgent cases within 1-3 days
- Some private insurers may take longer for high-cost treatments
- Many require extra review for surgeries or specialty drugs
- Busy periods can also slow things down.
Tip to speed things up: Follow each payer’s specific rules and submit through their online portals when possible.
4. How the Provider Submits and Follows Up
The clinic’s process matters a lot.
Faster approvals usually happen when providers:
- Submit requests electronically
- Check insurance coverage early
- Track authorization status daily
- Respond quickly to payer questions
Slower results often come from manual paperwork and delayed follow-ups.
Tip to speed things up: Having a team or specialist handle prior authorizations helps reduce delays. denials.
How the Prior Authorization Process Affects Approval Timelines
The length of time it takes to receive prior authorization is not only controlled by the insurance company. In most cases, the provider’s workflow plays a major role in whether approvals happen quickly or stretch into weeks.
Every step in the authorization process either speeds things up or creates delays.
1. Documentation Quality Has the Biggest Impact
Incomplete or unclear clinical documentation is the number one reason authorization requests stall. When diagnosis codes do not clearly support the requested service, or when progress notes are missing, insurers pause the review and ask for more information.
Each documentation request typically adds several extra business days to the timeline. In complex cases, repeated follow-ups can push approvals back by one to two weeks or more.
Clear medical necessity upfront is often the difference between fast approval and extended review.
2. Submission Method Influences Processing Speed
How the request is submitted also affects turnaround time.
Electronic portal submissions usually move faster because:
- Information is instantly received
- Required fields are validated automatically
- Tracking updates are available in real time
Faxed or phone requests often take longer to enter payer systems and are more likely to require follow-up due to missing data.
Practices using electronic workflows generally see approvals processed days faster than manual submissions.
3. Review Level Determines Timeline Length
Not all authorization requests receive the same type of review.
Simple services may pass through automated systems quickly.
High-cost or complex treatments are often routed to clinical reviewers or medical directors.
When medical director review or peer-to-peer discussions are required, timelines typically extend by several additional days.
The more clinical judgment involved, the longer the approval process tends to take.
4. Follow-Up Practices Prevent Stalled Requests
Many authorization delays happen because requests sit without updates.
Without regular tracking:
- Missing documentation requests go unnoticed
- Reviews stay pending longer than necessary
- Approvals expire before services are scheduled
Teams that follow up consistently often prevent multi-day or multi-week delays simply by keeping requests active in payer systems.
5. Expired or Incorrect Authorizations Restart the Process
Even after approval, timelines can reset if:
- The service is not scheduled within the authorized window
- Visit limits are exceeded
- Authorization numbers are entered incorrectly on claims
These issues often require reauthorization or corrections, adding days or weeks before payment can occur.
Best Practices to Reduce Prior Authorization Turnaround Time

Delays in prior authorization can be stressful for both patients and providers. The good news is that with the right approach, many approvals can be obtained much faster. Here are some proven ways to keep the prior authorization process moving and work toward faster prior authorization approval.
1. Submitting Complete and Accurate Requests
Before sending a request, double-check that every required form, test result, and medical note is included. Even small errors, like missing signatures or mismatched patient details, can cause prior authorization delays. Providers who create a checklist for each payer and train their staff on denial management best practices often see fewer rejections and faster responses.
2. Using Payer Portals or Electronic Submission
Many insurance companies now have secure online portals for prior authorization. Submitting electronically is usually quicker than fax or mail because it reaches the right department immediately. These systems often provide instant confirmation and tracking tools, helping the provider monitor progress without repeated phone calls. Combining electronic submission with early insurance eligibility verification can prevent delays before they start.
3. Tracking and Follow-Up Best Practices
Submitting a request is just the first step. The real speed comes from consistent follow-up. Assigning a team member to check request statuses daily ensures that any missing information is addressed right away. Using a follow-up log or task system can help avoid forgotten requests, which can otherwise lead to common medical billing denials or rescheduling patient care.
When providers stay organized and proactive, patients get the care they need sooner, and the practice avoids unnecessary billing issues.
Conclusion
Prior authorization timelines can vary depending on the insurer, the type of treatment, and how complete the request is. While some approvals move quickly, others take longer when additional reviews or documentation are needed. With the right workflows in place, many delays can be reduced.
Practices that stay organized, submit accurate information, and track requests closely tend to experience smoother approvals and fewer billing disruptions. Because the process is detailed and time-sensitive, many providers choose to use prior authorization services to manage approvals more efficiently.
If prior authorizations are creating backlogs, cancellations, or staff burnout, partnering with an experienced team can make a measurable difference. Our prior authorization services take the workload off your team while ensuring every request meets payer requirements from the start. With proactive tracking, thorough documentation, and real-time follow-ups, we help reduce delays, prevent denials, and keep your operations running smoothly.
Frequently Asked Questions
Find quick answers to common questions about this topic, explained simply and clearly.
How can I speed up my prior authorization?
Verify eligibility first, use payer portals for real-time submissions, attach complete clinical notes and correct CPT/ICD-10 codes, flag urgency when appropriate, and track status with alerts. Build specialty-specific templates and keep a payer rules l
How long does it take for insurance to approve prior authorization?
Timelines vary by payer and service. Many commercial plans decide in 2 to 5 business days. Urgent requests may be 24 to 72 hours. Complex imaging, specialty drugs, or surgery can take longer, especially if the payer requests more documentation.
Why would insurance deny prior authorization?
Common reasons include missing clinical criteria, wrong codes, lack of medical necessity based on payer policy, out-of-network provider, expired or inactive insurance, missing prior trials for step therapy, or late submission.
Why is it so hard to get a prior authorization?
Requirements differ by payer and plan, policies change often, and approvals depend on precise documentation that matches medical necessity rules. High call volumes and manual processes add delays. Standardizing intake, using checklists, and automating