What Is Unbundling in Medical Billing?
- Updated Date Jan 8, 2026
- Medical Billing
- Follow
Unbundling in medical billing is one of those behind-the-scenes issues that can create big problems if left unchecked. It happens when services that should be billed together are separated into multiple codes, leading to confusion, denials, or even compliance risks. In this blog, you will learn about:
- Bundling vs. Unbundling
- How Unbundling Happens in Coding
- The Role of NCCI Edits & CMS Rules
- Consequences of Unbundling
- Examples of Unbundling in Healthcare
- Unbundling vs. Other Fraudulent Practices
- How to Avoid Unbundling Errors.
What is unbundling in medical billing?
Unbundling in medical billing happens when services that should be billed together under one code are instead split and billed separately. This practice is a big concern because it can lead to overbilling, higher reimbursements than allowed, and even fraud investigations. Claims flagged for unbundling are often denied, which slows down payments and creates financial risk for providers. At the same time, payers face unnecessary costs, making unbundling an issue that affects both sides of the healthcare system.
Bundling vs. Unbundling

Bundling in medical billing means combining related procedures under a single CPT code, while unbundling separates them into multiple codes that should not be billed together. For example, when a patient receives a basic metabolic panel, the correct bundled code is CPT 80048, which covers all the lab tests included in the panel. If a provider instead bills the individual components like CPT 82310 (calcium test), CPT 82947 (glucose test), and CPT 84295 (sodium test) separately, that would be considered unbundling. This coding error or misuse inflates charges and may result in claim denials, overpayments, or compliance issues.
How Unbundling Happens in Coding
Unbundling happens when CPT codes are used the wrong way, often with the help of modifier codes. One of the most common issues is modifier 59, which is supposed to show when two services are truly separate but is sometimes misused to get extra payment. For example, a lab may bill each test in a basic metabolic panel individually instead of using the bundled code 80048. Sometimes this is an honest coding mistake, but other times it is done on purpose, which can lead to denied claims or even fraud investigations. For more understanding, you can explore our medical coding detailed guide.
The Role of NCCI Edits & CMS Rules
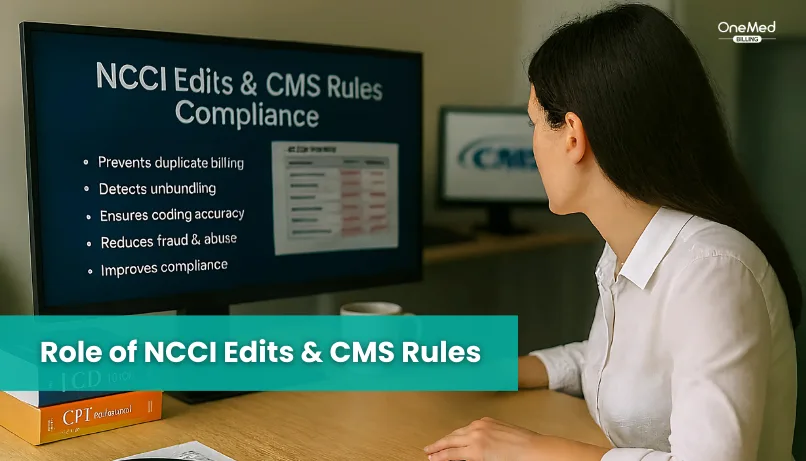
The National Correct Coding Initiative (NCCI), created by the Centers for Medicare & Medicaid Services (CMS), was designed specifically to prevent unbundling and other coding errors. NCCI edits act as built-in rules that stop providers from billing two codes separately when they are supposed to be bundled into one. In addition, Medically Unlikely Edits (MUEs) limit how many times a service can reasonably be billed for a single patient on the same day, which helps prevent duplicate or unbundled claims. Together, these safeguards reduce the chances of unbundling, protect providers from denials, and help payers avoid overpayments.
Consequences of Unbundling
Unbundling can have serious consequences for both providers and payers, and many of them carry long-term financial and compliance risks.
- Claims billed this way are often denied, which means revenue is lost and payments are delayed.
- If the claim is paid, insurers may later find the error and demand repayment or apply financial penalties.
- When unbundling appears deliberate, it may result in audits, fraud investigations, or legal action against the provider.
Examples of Unbundling in Healthcare
Unbundling appears in different areas of healthcare, and each situation creates risks for billing accuracy and compliance. Some real-world examples include:
- A laboratory runs a lipid panel, but bills each test, such as cholesterol, HDL, and triglycerides, separately instead of using the correct bundled code 80061.
- During cataract surgery, services like lens insertion and post-operative care are billed individually, even though they are part of the global surgical package.
- A radiology clinic charges separately for each MRI sequence of the same knee rather than billing the complete MRI exam under the single bundled code.
- In one compliance audit, a hospital was found to be billing wound debridement and dressing changes as separate procedures, which led to repayment demands and closer monitoring.
Unbundling vs. Other Fraudulent Practices
Unbundling is often grouped with other billing fraud practices, but each has its own definition and risks. Understanding the differences helps providers recognize why all three are closely monitored in audits.
Upcoding happens when a provider bills for a higher level of service than what was actually given. For example, billing for a 60-minute office visit when the patient was only seen for 15 minutes is considered upcoding.
Duplicate billing occurs when the same service is billed more than once. An example is submitting two claims for the same X-ray performed on the same date.
Unbundling is different because it involves splitting services that should be billed together under one code. For instance, charging separately for incision, closure, and anesthesia during surgery instead of using the single bundled surgical code.
While these practices vary, they all share the risk of inflating reimbursement and triggering compliance concerns, making them a top priority for payers and regulators.
How to Avoid Unbundling Errors
Preventing unbundling requires a mix of strong internal processes, accurate coding practices, and strict compliance with payer rules. Many errors happen because staff are not fully trained on coding updates, don’t have complete knowledge about common denial codes, or rely on outdated software, which makes mistakes more likely. Some of the best ways to avoid errors include:
• Providing regular training for coding staff so they stay updated on CPT, modifiers, and bundling guidelines. Many providers also choose to outsource medical coding services to ensure compliance and accuracy.
• Using modern billing software that applies NCCI edit checks to catch mistakes before claims are submitted.
• Conducting routine internal audits to identify patterns of unbundling and correct them quickly.
• Following CMS and payer guidelines closely to ensure services are billed correctly and in compliance with regulations.
Conclusion
Unbundling may look like a small coding choice, but the impact it carries is anything but small. It can quietly drain revenue, create unnecessary conflicts with payers, and place a provider’s compliance record under the spotlight. The real safeguard is not after-the-fact corrections, but a proactive approach where coding accuracy, technology checks, and continuous staff training work together. By staying ahead of these risks, providers turn billing compliance from a burden into a strength that protects their practice and builds trust across the healthcare system.
Frequently Asked Questions
Find quick answers to common questions about this topic, explained simply and clearly.
What is an example of unbundling in medical billing?
An example is billing cholesterol, HDL, and triglycerides separately instead of using CPT 80061 for a lipid panel.
How to tell if a CPT code is bundled?
You can tell by checking CMS NCCI edits or using coding software with built-in bundling rules.
What tools or rules exist to stop unbundling?
CMS uses the National Correct Coding Initiative (NCCI) edits and Medically Unlikely Edits (MUEs) to flag and prevent unbundled claims. These systems act as safeguards before payments are made.
What’s the difference between unbundling and upcoding?
Unbundling means splitting services that should be grouped under one code, while upcoding means billing for a higher-level service than what was provided. Both are considered risky billing practices and may trigger audits.
Are all unbundling cases fraudulent?
No, not all unbundling cases are fraudulent. Some are honest coding errors caused by lack of training or outdated systems, but intentional unbundling is considered fraud.