What Is Prior Authorization? - Detailed Guide for Providers
- Updated Date January 17th, 2026
- Prior Authorization
- Follow
Prior authorization is a step in healthcare where a provider must get approval from a patient’s insurance company before providing certain treatments, tests, or medications. Think of it as a “green light” from the payor. Without it, the insurance company may refuse to pay, leaving the patient with an unexpected bill.
In recent time, this process matters the most. Healthcare costs keep rising, and payors want to make sure every service is medically necessary and follows the rules. At the same time, patients depend on quick approvals to avoid delays in care. Prior authorization, when done right, helps control costs, keeps providers compliant with insurance policies, and makes sure patients get timely access to the treatments they need.
What Is Prior Authorization?
Prior authorization is a review process used in healthcare where a provider must obtain approval from the patient’s insurance company before moving forward with certain services, tests, or prescriptions. Depending on the service and plan rules, different types of authorization may apply. The goal is to confirm that the care being requested is medically necessary and covered under the patient’s health plan.
This process is most often required for high-cost services such as advanced imaging (like MRIs), surgeries, or specialty medications. For example, if a patient needs a back surgery, the provider must send clinical notes and test results to the payor. Only after the request is approved can the surgery be scheduled with confidence that insurance will help cover the expense.
Prior authorization may also be called pre-authorization, pre-certification, or pre-approval. These terms are often used interchangeably, but understanding how precertification and preauthorization differ in certain situations can help you avoid confusion.
Why Insurance Companies Require Prior Authorization

Insurance companies use prior authorization as a safeguard to manage healthcare spending and make sure care is appropriate. While the process can sometimes feel like a barrier for providers and patients, payors see it as an important tool for controlling risk and protecting resources.
Cost Containment
As healthcare costs rise each year, prior authorization helps payors manage expenses by reviewing costly tests, surgeries, and medications before approval, covering only what is medically necessary to prevent wasteful spending and keep patient premiums more stable.
Ensuring Medical Necessity
Payors use prior authorization to confirm that a test or treatment is truly necessary by requiring providers to submit clinical evidence, such as patient history or lab results, so that care follows medical guidelines instead of unnecessary or duplicate services.
Reducing Misuse of High-Cost Procedures and Drugs
Some services, like MRIs, advanced surgeries, or specialty medications, are not only expensive but can also be overused. Prior authorization plays a crucial role in preventing misuse by making sure that medical services or medications are only approved when there's a solid justification. This protects patients from unnecessary procedures and helps maintain the long-term sustainability of the healthcare system.
Protecting Payors Risk
Insurance companies pool risk across many members, and prior authorization helps protect that pool by preventing payment for services that are unnecessary or ineffective, limiting financial exposure while keeping resources available for patients who genuinely need them.
The Prior Authorization Process Step by Step

The prior authorization process may look different from one payor to another, but most follow the same basic flow. It begins when a provider identifies the need for a service and ends with the insurance company’s decision to approve, deny, or request more details. Below is a clear step-by-step outline of how it usually works.
Step 1: Provider identifies the need for a service or drug
The doctor decides a patient needs a specific test, treatment, surgery, or medication. The care team checks the patient’s insurance plan to see if prior authorization is required for that service. If approved, providers submit clinical notes to show why the service is medically necessary.
Step 2: PA request submitted with documentation
The clinic submits a prior authorization request to the insurance company. This can be through a payor portal, fax, or EHR integration. The request includes the diagnosis code, procedure or drug code, and supporting records.
Typical documents include recent visit notes, lab or imaging results, past treatments tried, and the treatment plan.
Step 3: Payor Reviews the Request
The insurance company reviews the request as per rules and clinical guidelines. A clinical reviewer from the insurance company evaluates medical necessity, checks for lower-cost alternatives, and may ask the provider for clarification or additional records if needed.
Step 4: Approval, denial, or request for more information
After review, the payor issues one of three outcomes:
- Approval if the service meets criteria.
- Denial if it does not meet the criteria or is not covered.
- Request for more information if details are missing or unclear.
If denied, the provider has to correct the request, submit more documents, or file an appeal.
Step 5: Patient and provider notified
The decision is shared with both the clinic and the patient, if approved, the clinic schedules the service and records the authorization number with its validity dates; if denied or delayed, the clinic informs the patient of next steps, which may include providing additional information, choosing an alternative that is covered, or simply wait, depending on the time prior authorization approval can take before moving forward with treatment.
Common Services and Treatments That Require Prior Authorization
Not every medical service needs prior authorization, but many high-cost or high-risk treatments do. Insurance companies typically require it when the service is expensive, has the potential for overuse, or involves patient safety concerns. Some of the most common examples include:
1. Imaging Tests
Advanced imaging, such as MRI, CT, and PET scans, often requires prior authorization. These tests are costly, and payors want to ensure they are necessary before approving them.
2. Surgeries and Hospital Admissions
Most planned surgeries and hospital admissions require prior authorization, allowing payors to confirm the procedure is appropriate and that less invasive options were considered first.
3. Specialty Medications
Drugs such as biologics, injectables, or other specialty therapies are usually subject to prior authorization. These treatments can be very expensive and may require proof that standard medications were tried first.
4. Behavioral Health Services
Certain mental health and substance use treatments may need prior authorization. Payors often require it for inpatient behavioral health stays, intensive outpatient programs, or specialized therapies.
5. Out-of-Network Care
When a patient chooses a provider or hospital that is outside their insurance network, prior authorization is often required. This gives the payor a chance to review the request and decide if it qualifies for coverage.
Challenges of Prior Authorization in Healthcare

While prior authorization is meant to control costs and ensure appropriate care, it often creates significant challenges for both providers and patients.
Administrative Burden
Managing prior authorizations requires a heavy load of paperwork and back-and-forth communication with payors. Staff must track requirements, submit forms, and follow up repeatedly, which pulls time and resources away from the provider, distracting the main focus.
Delays in Patient Care
Prior authorization can slow down access to necessary treatments. Patients may have to wait days or even weeks for approval before starting therapy or undergoing a procedure. According to the American Medical Association (AMA), 94% of physicians report that prior authorization delays patient care, which can worsen health outcomes.
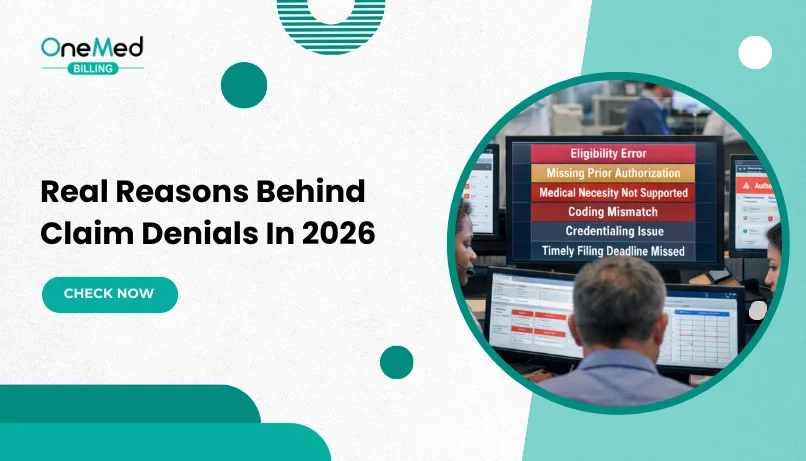
Denials and Revenue Loss
Even when a service is medically necessary, prior authorization can still be denied if the documentation is missing or incomplete. This not only delays or disrupts patient care, putting the patient’s health at risk, but also creates financial losses for providers, who are then forced to either go through a lengthy appeal process or risk not getting paid at all.
Lack of Standardization
Every insurance company sets its own prior authorization rules. Requirements vary widely by payor, making it difficult for providers to keep up and adding complexity to an already burdensome process.
Patient Frustration
Patients often feel confused by the prior authorization process. Limited transparency, long wait times, and unexpected denials can leave them frustrated, anxious, and distrustful of both their payor and provider.
The Role of Prior Authorization in Medical Billing and RCM
- Prior authorization is a critical step in the revenue cycle. Since it happens before treatment is provided, it often determines whether the claim will be approved and how smoothly the provider will get paid.
- Starting point in the billing cycle - Prior authorization acts as an early checkpoint. If approval is secured, the claim moves forward with fewer obstacles. If it is missed, the entire billing process can break down.
- Keeps payments moving - Clean and timely approvals mean insurance companies process claims faster. This gives providers a steady cash flow and reduces the financial stress caused by late reimbursements.
- Mistakes lead to costly denials - Errors such as missing paperwork, wrong codes, or delays in submission often result in denials. Each denial forces staff to resubmit or appeal, which wastes time and may lead to lost revenue.
- Essential for revenue cycle management - Every part of RCM is connected. A weak prior authorization process can cause scheduling delays, disrupt patient care, and damage the financial health of a practice. This is why many providers treat PA as a critical part of their overall billing strategy.
Tips to Streamline the Prior Authorization Process
Prior authorization can be time-consuming, but with the right strategies, providers can reduce delays and improve approval rates. Here are some proven tips:
1. Train Staff on Payor-Specific Requirements
Every insurance company has different rules. Training staff to understand payor-specific guidelines helps reduce mistakes and ensures requests are submitted correctly the first time.
2. Use Electronic Prior Authorization (ePA) Tools
ePA tools allow clinics to submit and track requests digitally. This speeds up communication with payors, reduces paperwork, and shortens turnaround times.
3. Build Payor Rule Libraries in Your PM System
Creating a library of prior authorization rules inside your practice management system helps staff know exactly when PA is needed. This prevents missed authorizations and reduces denials.
4. Track and Analyze Denials to Prevent Repeats
Review denial patterns regularly to find out why requests are being rejected. Fixing the root causes, such as missing documents or coding errors, helps prevent the same problems from happening again.
5. Consider Outsourcing Prior Authorization Services
For busy practices, outsourcing can be a smart option. Specialized teams handle the entire process, from submitting requests to following up with payors, allowing providers to focus on patient care while reducing the administrative load.
Future of Prior Authorization in Healthcare
The prior authorization process is changing as technology and policy reforms aim to reduce the burden on providers and patients. Several trends are shaping the future of PA:
Growth of Automation and AI in PA
Automation and artificial intelligence are being used to speed up prior authorization. AI tools can review clinical data, match it with payor rules, and flag missing information before a request is submitted. This reduces errors, shortens approval times, and lowers the administrative workload for staff.
CMS and Payor-Driven Reforms
The Centers for Medicare & Medicaid Services (CMS) and commercial payors are pushing for reforms to simplify the prior authorization process. New rules aim to improve transparency, require faster response times, and cut down on unnecessary delays. These changes are designed to give providers more time for patient care instead of paperwork.
The Move Toward Real-Time Electronic PA Approvals
Electronic prior authorization (ePA) is expected to become the standard, with real-time approvals through systems that connect providers, payors, and pharmacies. This shift will speed up patient access to care, reduce frustration, and move prior authorization toward a more efficient, technology-driven future that balances cost
control with timely treatment.
Outsourcing Prior Authorization: Should You Consider It?

For many practices, prior authorization has become one of the biggest challenges in medical billing. The constant paperwork, payor follow-ups, and denial management often overwhelm in-house teams and take valuable time away. In situations like this, outsourcing prior authorization can be a practical solution.
You may need outside support if your practice is dealing with a growing backlog of pending authorizations, staff burnout from handling excessive paperwork, or high denial rates caused by incomplete or late submissions. Delays in treatment because approvals take too long are also a strong sign that it may be time to consider outsourcing.
Conclusion
Prior authorization plays an important role in today’s healthcare system. For providers, it determines whether claims are paid smoothly or denied. For payors, it is a safeguard that helps control costs and ensure treatments are medically necessary. And for patients, it can be the difference between getting timely access to care or facing frustrating delays.
While the process often creates a heavy burden for staff and can delay treatment, it remains a necessary step in protecting both financial resources and clinical outcomes. The challenge for practices is not whether prior authorization should exist, but how to manage it in a way that minimizes disruption.
By adopting smarter processes, training staff, using electronic tools, or even outsourcing, providers can ease the workload and reduce denials. Taking these steps allows practices to protect revenue, support staff, and most importantly, give patients quicker access to the care they came for.
Frequently Asked Questions
Find quick answers to common questions about this topic, explained simply and clearly.
What is prior authorization in simple terms?
Prior authorization is when your doctor asks your insurance company for approval before giving certain tests, treatments, or medications. It makes sure the service is covered and medically necessary.
Does prior authorization mean insurance will pay?
Getting prior authorization usually means your insurance will cover the service, but it does not guarantee payment. Claims can still be denied later if other billing rules are not followed.
How long does prior authorization usually take?
The time varies by payor and service. Some approvals are given within 24–48 hours, while others, especially for complex treatments, may take several days or even weeks.
What services require prior authorization?
Common services include advanced imaging (like MRI or CT scans), surgeries, hospital admissions, specialty medications, behavioral health treatments, and out-of-network care.
Can a prior authorization be denied, and why?
Yes. Prior authorization can be denied if the service is not covered by the plan, if it lacks medical necessity, or if the request has missing or incorrect documentation.